Targeting Complement System May Help Halt Autoimmune Hemolytic Anemia, Study Suggests
A small molecule targeting a protein of the complement system — a large group of plasma proteins that normally react with one another to fight infection — may help prevent the destruction of red blood cells that characterizes autoimmune hemolytic anemia (AIHA), a study suggests.
The study “Complement C3 inhibition by compstatin Cp40 prevents intra- and extravascular hemolysis of red blood cells” was published in the journal Haematologica.
In autoimmune hemolytic anemia (AIHA), the immune system recognizes red blood cells as foreign, and targets them for destruction. Cold agglutinin disease (CAD) is a form of AIHA.
The first-line treatment for AIHA uses immunosuppressants that aim to reduce the production of autoantibodies. However, this strategy is not effective in all AIHA patients, and can result in uncontrolled anemia, or the loss of red blood cells. In these cases, patients receive blood transfusions — but the autoantibodies may react against the donor red blood cells.
Now, researchers investigated the therapeutic potential of targeting the complement system, a set of more than 30 blood proteins that form part of the body’s immune defenses. The investigators used a small peptide called compstatin (Cp40) to avoid red blood cells breakdown in AIHA. In particular, Cp40 targets the complement C3 molecule, a protein that attaches to the surface of red blood cells, tagging them for destruction.
To test this alternative treatment, the team used blood from AIHA patients that tested positive for deposits of the C3 molecule on red blood cells. Adding the Cp40 to the samples almost entirely cleared the accumulations of C3b from the cells, the study showed.
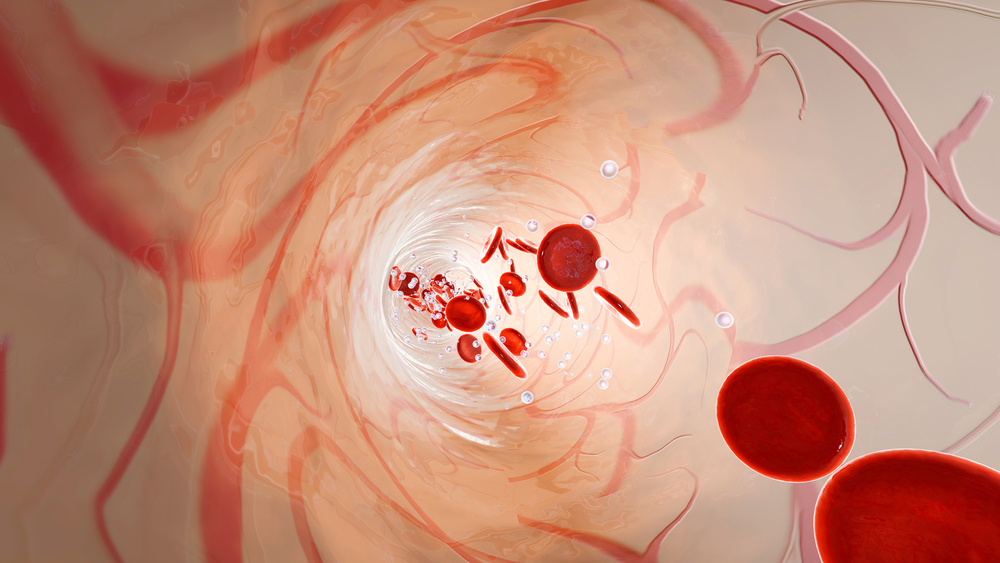
The researchers also saw that adding Cp40 prevented hemolysis — ruptured red blood cells — by halting the formation of a structure called membrane-attack complement (MAC). The MAC disrupts the cell membrane, leading cells to burst. The destruction of the red blood cells inside blood vessels is called intravascular hemolysis.
The blocking of red blood cell destruction was similar to that seen with Alexion’s Soliris (eculizumab), an FDA-approved therapy targeting the complement system. Soliris stops the terminal part of the complement cascade, namely the C5 protein, and also blocks MAC formation.
Next, researchers investigated whether Cp40 had an effect on red blood cells’ phagocytosis, the process by which immune cells — called macrophages — “eat” large particles to destroy them. This is called extravascular hemolysis, since red blood cells are destroyed by macrophages in the spleen or liver, a process that is not stopped by Soliris.
Indeed, Cp40-mediated inhibition of the C3 complement also reduced the ability of macrophages to “eat” and destroy the red blood cells.
These findings suggest that Cp40 can inhibit red blood cells destruction by targeting the C3 complement protein.
Previous studies had shown that inhibition of complement C5 had a beneficial effect for people CAD. But these findings “show that complement regulation by Cp40 can be even more beneficial since both intra- and extravascular hemolysis are prevented,” the researchers said.
“Together, we conclude that Cp40 is a promising new treatment for complement-mediated AIHA” the study concluded.