High-temperature plasmapheresis checks hemolysis in secondary CAD
Report offers example of managing blood cell death during procedure
Maintaining a high temperature with the equipment used for plasmapheresis therapy in people with cold agglutinin disease (CAD), along with the environment and patients, may help prevent the risk of red blood cell clumping and destruction during the procedure, a new case report suggests.
“Although our approach still has room for improvement, our management protocol appears to be an effective treatment modality for” CAD patients experiencing signs of red blood cell destruction, or hemolysis, during plasmapheresis, the researchers wrote in “Successful Management of Total Plasma Exchange for Hemolytic Cold Agglutinin Disease,” which was published in Internal Medicine.
CAD is an autoimmune disease caused by the production of self-reactive antibodies, called cold agglutinins, that bind to red blood cells at cold temperatures. This causes the cells to clump together and be flagged for destruction by the immune system, resulting in anemia, and CAD symptoms. Anemia refers to lower than normal red blood cell levels or deficient levels of hemoglobin, the protein in the cells that helps carry oxygen throughout the body.
When CAD occurs due to an underlying condition, such as a blood cancer, an infection, or another autoimmune disease, it’s called secondary CAD.
CAD patients are at a higher risk of complications during surgeries that require the body to be maintained at low temperatures. Because of this, several preventive measures to increase a patient’s temperature or that of the equipment used are implemented in such scenarios.
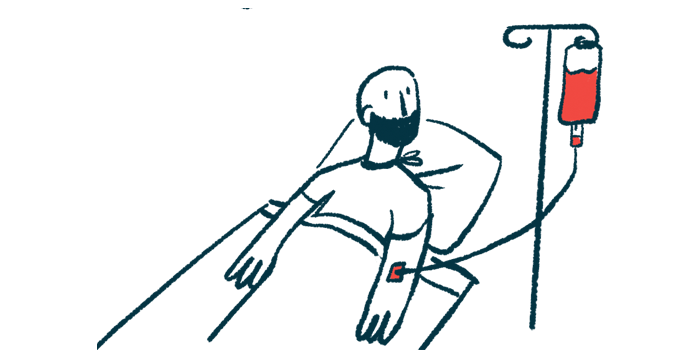
Plasmapheresis, or plasma exchange, is a blood-cleaning procedure to reduce levels of cold agglutinins and may help ease CAD symptoms. It involves collecting the patient’s blood into a machine that removes its plasma, or liquid portion, where antibodies and other proteins are. The same amount of fresh, healthy plasma is then mixed with the patient’s blood cells for infusion back into the patient.
But if cold agglutinins react at room temperature, red blood cells can clump in the plasmapheresis equipment. It’s therefore recommended that the procedure be conducted under high temperatures for these patients.
Managing hemolysis
“However, there are no reports of hemolysis during [plasmapheresis] and its management in patients with CAD,” wrote researchers at the Kyushu University Hospital, Japan who described the case of a 41-year-old man with secondary CAD who developed hemolysis during plasmapheresis.
The man was first seen at the hospital with shortness of breath on exercise and general fatigue. These symptoms were accompanied by a dry cough, brown urine, and jaundice, a condition where the skin and the whites of the eyes turn yellow due to bilirubin, a marker of hemolysis, building up in the blood.
Blood work revealed low hemoglobin and elevated levels of bilirubin and lactate dehydrogenase, another hemolysis marker.
A positive direct Coombs test, which assesses whether antibodies and other immune proteins are attached to red blood cells, and the detection of cold agglutinins confirmed a CAD diagnosis.
Further tests excluded infection and pointed to a rare blood cancer called lymphoplasmacytic lymphoma/Waldenstrom’s macroglobulinemia (LPL/WM), as the cause of CAD.
The man was diagnosed with CAD secondary to LPL/WM. At this time, several blood parameters had improved or normalized. However, after a first round of chemotherapy to treat his blood cancer, he presented severe hemolysis and anemia, which precluded more chemotherapy.
He was given corticosteroids to control his CAD, but this had no effect so he was referred for plasmapheresis. To prevent the risk of hemolysis during the procedure, the temperature in the room was set at 30 C (86 F) and a blood warmer was used.
Within 10 minutes, however, his red blood cells started to clump together and hemolysis was detected in the device that temporarily draws the blood out of the body, impairing blood flow. The procedure was halted.
Tests showed the man’s blood started to show red blood cell clumping at 34 C (93.2 F). The clumping was resolved by warming it to 36 C (96.8 F).
He was resubmitted to plasmapheresis. His body temperature was increased with an electric blanket, and the plasmapheresis machine and its tubes were kept at a higher temperature. Under this high-temperature setting, the man completed three plasmapheresis rounds without any complications. His blood parameters were normalized and he was able to receive chemotherapy after the last round of plasmapheresis without any severe complications.
“Although our management methodology is still quite primitive and there remains room for improvement […] our method appears to be an expedient method,” the researchers wrote. “Further studies are required to improve the performance of [plasmapheresis] in CAD patients.”