Thrombotic events common in adults with CAD, AIHA: Study
Blood clots more likely in patients experiencing 5 or more hemolytic attacks
Written by |
Thrombotic events (TE), or the blockage of blood flow due to blood clots, are relatively common among adults with cold agglutinin disease (CAD) and other forms of autoimmune hemolytic anemia (AIHA), according to a study in France.
Researchers also found that experiencing five or more hemolytic attacks marked by accelerated red blood cell destruction is associated with an increased risk of thrombotic events in people with AIHA.
“Given the prevalence of thromboembolic complications in AIHA, it is critical that clinicians remain vigilant and proactive in managing the TE [thrombotic event] risk in AIHA,” researchers wrote.
The study, “Prediction of thrombotic events in patients with autoimmune hemolytic anemia: a multicenter retrospective observational study,” was published in the Journal of Thrombosis and Thrombolysis.
AIHA patients have increased risk of thrombotic events
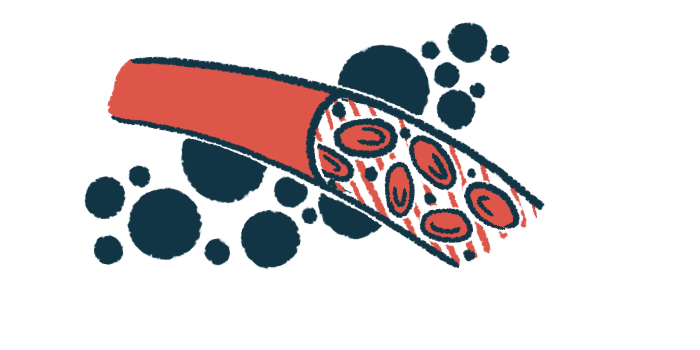
AIHA occurs when the immune system produces self-reactive antibodies that mistakenly attack red blood cells, marking them for destruction. This process, known as hemolysis, causes anemia, in which there are not enough red blood cells supplying oxygen to the body. This, in turn, leads to AIHA symptoms.
The temperature range under which self-reactive antibodies bind to red blood cells dictate the type of AIHA. CAD is the diagnosis when binding occurs at cold temperatures. In warm AIHA, warmer temperatures trigger this process. Mixed forms of AIHA include binding at both cold and warm temperatures.
AIHA can also be classified depending on the cause. If underlying conditions, such as viral infections or other autoimmune diseases, are the likely cause, it is considered secondary. Primary AIHA covers cases for which the cause is unknown.
Previous studies have reported that people with AIHA have an increased risk of TE, particularly of venous thromboembolism (VTE), a type of TE in which blood clots block veins.
Less evidence exists regarding links between AIHA and arterial thromboembolism (ATE). ATE is similar to VTE, but occurs in the arteries that carry oxygen-rich blood through the body, rather than the veins, which carry oxygen-poor blood back to the heart.
Clinical guidelines for prevention and management of TE associated with AIHA aren’t comprehensive, according to the research team. However, “the identification of specific risk factors in AIHA is paramount to enhance patients’ management and survival,” they wrote.
French researchers analyzed records of 88 adults
To address this need, the team of researchers in France retrospectively analyzed medical records from 88 adults with AIHA, including 72 with warm AIHA and 13 with CAD (seven with primary disease and six with secondary disease).
Participants, seen at three French centers, had a mean age of 63.7 when diagnosed, and had records from a mean of 3.9 years after diagnosis.
During follow-up, 30 TEs occurred in 22 AIHA patients (25%), including three out of the 13 CAD patients (23.1%). Specifically, 16 patients experienced 19 VTEs and seven patients experienced 11 ATEs.
Clinicians should be aware of this high risk of TE in AIHA, particularly during hemolytic phases, especially when they are repeated.
These findings “provide further evidence supporting that patients with AIHA are at very high risk of TE complications, either arterial, venous or both,” the team wrote.
Statistical analyses showed that the only factor significantly associated with overall risk of TE was having five or more hemolytic attacks. Individuals who reached this threshold had nearly seven times the risk of TE than those with fewer recorded events. However, there was no significant link between the intensity of the hemolytic activity and TE risk.
“Clinicians should be aware of this high risk of TE in AIHA, particularly during hemolytic phases, especially when they are repeated,” the researchers wrote.
In addition, having primary warm AIHA or a history of VTEs were each significantly associated with a threefold increased risk of VTE, while having a procedure to remove the spleen was linked to seven times higher risk.
Assessment scale shows relationship with VTE risk in outpatient group
A scale intended to assess risk of VTE in inpatient hospital settings, called the Padua prediction score, also showed a relationship with VTE risk in this outpatient AIHA group. Participants who experienced a VTE during the study had higher median scores than those who didn’t, indicating higher predicted risk. Two items on the Padua prediction score — history of VTE and reduced mobility — drove most of this risk.
Further analyses showed that for ATE, being 80 years or older at the time of diagnosis and having at least three cardiovascular risk factors significantly increased risk, by nearly nine times each.
Most participants (87.5%) were alive after one year, with the survival rate dropping to 58% at the end of follow-up. Notably, “TE complications accounted for 9.4% of the deaths, but infections remained the leading cause of mortality, consistent with other studies,” the team wrote.
Without a control group, it wasn’t possible for the researchers to assess TE risk in people with AIHA relative to people without the condition. Although the total number of TEs didn’t allow for more complex statistical analysis, the team noted that this is one of the largest studies of its kind given the rarity of AIHA.
“The findings from this study could serve as a basis for future prospective [follow-up] trials, which could help validate these observations and develop a more standardized approach to manage the thrombotic risk in AIHA patients,” the researchers wrote.