Subclinical CAD Identified In 2 Patients With COVID-19
Both patients had CAD antibodies, but no signs of red blood cell destruction or thrombosis

Patients who develop cold agglutinin antibodies after COVID-19 infection won’t always show overt signs of cold agglutinin disease (CAD), a case report suggested.
Two patients with COVID-19 at a clinic in Japan had high levels of the antibodies, but didn’t show signs of red blood cell destruction (hemolytic anemia) or blocked blood flow (thrombosis). The clinical significance of cold agglutinins in COVID-19 patients remains to be determined, the researchers noted.
The case report, “Cold agglutinin anti-I antibodies in two patients with COVID-19,” was published in the Journal of Clinical and Laboratory Analysis.
CAD is a rare condition wherein the immune system attacks red blood cells at cold temperatures. These attacks are mediated by antibodies called cold agglutinins, which bind to red blood cells, causing them to clump together and ultimately die. This means that not enough red blood cells are available to carry oxygen throughout the body, leading to anemia.
Secondary CAD, also known as cold agglutinin syndrome, develops as a result of an underlying health condition, such as cancer, autoimmune disorder, or infection.
It’s been reported to occur in several patients with COVID-19, most of whom developed the characteristic signs of CAD, namely hemolytic anemia, which occurs when red blood cells are destroyed faster than they can be produced, and the production of cold agglutinins.
This case report concerned two patients, a 64-year-old man and a 76-year-old woman, who were seen at the researchers’ hospital in Japan.
The man, who came to the hospital with a fever, was diagnosed with COVID-19 and admitted. He developed low oxygen six days later and required mechanical ventilation. He was treated with dexamethasone, tocilizumab, and piperacillin-tazobactam.
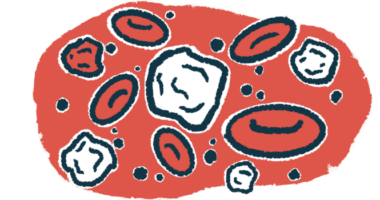
Clinicians looked at a smear of his blood under a microscope because lab tests showed he had a high concentration of hemoglobin — the protein in red blood cells that carries oxygen — in his red blood cells.
On the smear, red blood cell agglutination, or clumping, was observed. Lab testing revealed low zinc levels and macrocytic anemia — a condition marked by abnormally enlarged red blood cells that do not function normally — but no signs of hemolytic anemia.
A Coombs test was done to look for cold agglutinin antibodies, which were found at high levels. The test was positive for C3b/C3d, an immune system molecule known to be involved in CAD autoimmune attacks.
He was given zinc supplementation, which improved his hemoglobin levels. He was tapered off ventilation after treatment and was discharged home after 38 days in the hospital, and his cold agglutinin levels dropped to near normal range.
The woman reported to the hospital six days after testing positive for COVID-19 with low oxygen levels. She was treated with dexamethasone and remdesivir, after which her pneumonia improved, but she developed a urinary tract infection.
Like the first patient, she had high a hemoglobin concentration and a blood smear showed red blood cell agglutination. She tested positive for cold agglutinins and C3b/C3d. On the first visit following her discharge from the hospital, her cold agglutinin levels declined.
Researchers collected blood samples from each patient and tested them to determine which type of cold agglutinin antibodies were present.
Findings suggested antibodies in both belonged to a class of IgM antibodies normally released by the immune system to fight off infections. Specifically, researchers believed the antibodies to be anti-I.
The findings show subclinical CAD can occur after COVID-19 infection.
“Clinical manifestations might not be present because the two patients had no exposure of cold stimulate,” the researchers wrote. The female patient was admitted in springtime and the male in the winter, but he stayed in a warm room, according to researchers.
Given a lack of clear significance of cold agglutinins in COVID-19 patients, future studies will need to clarify this relationship, the research team noted.