Phase 3 Data Support Safety, Efficacy of Sutimlimab in Treating CAD
The investigational therapy sutimlimab prevented hemolysis, significantly increased hemoglobin, and improved the quality of life in patients with cold agglutinin disease (CAD), according to data from a Phase 3 clinical trial.
The results will be presented at the Annual Meeting of the American Society of Hematology in December, in a presentation titled “Inhibition of Complement C1s with Sutimlimab in Patients with Cold Agglutinin Disease (CAD): Results from the Phase 3 Cardinal Study.”
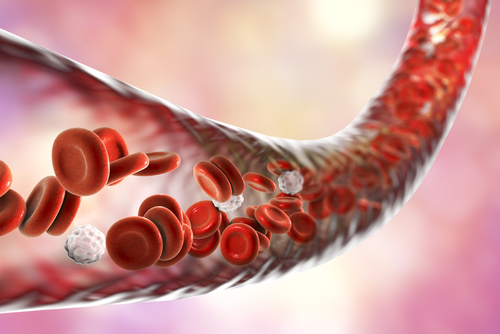
Sutimlimab (formerly BIVV009) is an antibody that selectively binds to and blocks the activity of C1s, a protein with a central role in the so-called classical complement pathway. Activation of this pathway is a cause of CAD hemolysis, which refers to destruction of the red blood cells responsible for storing and transporting the oxygen-carrying protein hemoglobin (Hb).
The Phase 3 CARDINAL study (NCT03347396) enrolled 24 people with CAD who had low levels (10 g/dL or less) of hemoglobin and who had received at least one blood transfusion in the six months before enrollment. The trial was open-label, with all participants receiving the active treatment (sutimlimab), and no placebo given. The trial was funded by Sanofi, the company that is developing sutimlimab.
Sutimlimab was given by intravenous (into a vein) infusion every week for the first two weeks, then every other week for the remaining 26 weeks, at doses that depended on the individual’s weight. Patients weighing less than 75 kg received a 6.5 g dose, while patients weighing 75 kg or more received a 7.5 g dose.
This trial is divided into two parts: part A aims to determine whether the therapy can increase hemoglobin levels to greater than or equal to 12 g per dL (the accepted normal range of blood hemoglobin level), or increase hemoglobin by 2 g/dL or more from baseline, and also make blood transfusions unnecessary for the CAD patients from weeks 5 to 26. Part B aims to study the treatment’s long-term safety and tolerability.
The results reported here correspond to the first part of the study.
The trial participants were 62.5% female, and their average age was 71.3 years. Twenty-two participants completed the 26-week trial; two withdrew for reasons unrelated to the treatment.
The primary endpoint, or goal, of this part of the trial was an increase in Hb with no need for additional blood transfusions.
The trial met its primary goal in 13 patients. Hb increased rapidly following the first treatment, with an average increase of 1.2 g/dL by week one and 2.3 g/dL by week three. At the end of the trial, average Hb had increased by 2.6 g/dL, such that the average Hb level was higher than 11 g/dL. (Prior to starting on sutimlimab, the patients’ average Hb level was 8.6 g/dL.)
Overall, 20 of the participants (83.3%) experienced an increase in Hb level of at least 1 g/dL. Furthermore, 17 participants (70.8%) did not require blood transfusions from weeks 5 to 26.
Additionally, quality of life improved which was reflected in significant and clinically relevant increases (10.9 points on average) in scores on the Functional Assessment of Chronic Illness Therapy Fatigue Scale.
Seven participants experienced a serious adverse event during treatment; however, none of these events were deemed related to sutimlimab. There was one death, due to liver cancer, which was also deemed unrelated to the treatment.
All 22 participants who completed the 26-week trial are now enrolled in an extension trial (part B).
“These pivotal data demonstrate the potential of sutimlimab as a first-in-class targeted treatment for this chronic and debilitating rare blood disorder,” said John Reed, MD, PhD, global head of research and development at Sanofi, in a press release.