IL-23 inhibitor may have therapeutic potential in AIHA: Case study
Complete remission seen for woman, 42, treated for another disorder

A woman with a mixed form of autoimmune hemolytic anemia (AIHA), who was having only temporary responses to standard treatment, experienced complete disease remission after being given an interleukin-23 (IL-23) inhibitor for a separate condition, a case study shows.
IL-23 inhibitor therapies are used for other inflammatory diseases, but have not yet been investigated as a potential AIHA treatment. Researchers believe this “fascinating case” warrants additional studies to probe the therapeutic potential of such treatment for all forms of AIHA, including cold agglutinin disease (CAD).
“Though we recognize these findings are retrospective and associative, further studies are needed for potential therapeutic avenue,” the scientists wrote.
This U.S. patient with treatment-resistant AIHA was given the therapy after a bout of psoriasis.
The case report, “Possible role of IL-23 inhibitor in autoimmune hemolytic anemia,” was published in the European Journal of Haematology.
Patient given IL-23 inhibitor to treat psoriasis
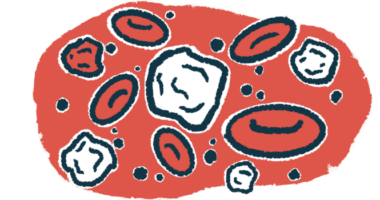
AIHA refers to a group of rare autoimmune diseases in which the immune system produces self-reactive antibodies that attack and destroy red blood cells.
It can be classified as CAD, warm AIHA, and mixed AIHA, depending on whether the antibodies bind more easily to red blood cells at lower temperatures — known as cold agglutinins — or higher temperatures. The mixed form has both antibody types.
The loss of red blood cells that characterizes all AIHA types leads to anemia and deprives tissues of oxygen, which is carried by hemoglobin, a protein in these cells. The disorder can cause fatigue and pain.
The main goal of treating AIHA is to reduce hemolysis and increase red blood cell production to ensure hemoglobin levels are normalized. Standard therapy includes immunosuppressing medications such as steroids like prednisone and rituximab, which works by killing the immune B-cells responsible for producing self-reactive antibodies.
Still, some patients become resistant to treatment, resulting in persistent symptoms that are poorly managed.
Recent research has suggested a role for the pro-inflammatory molecule IL-23 in AIHA. Its release is thought to promote the activation of T-helper 17 cells, a family of immune cells identified as harmful in a variety of autoimmune conditions.
IL-23 inhibitor therapies have shown beneficial effects in inflammatory diseases like psoriasis, an autoimmune skin condition. Risankizumab, sold under the brand name Skyrizi, is one such treatment approved for psoriasis patients.
Now, researchers at the University of Texas Southwestern Medical Center reported the case of a 42-year-old woman with mixed AIHA who, despite receiving standard treatment, achieved full remission only after being given risankizumab treatment for her psoriasis.
IL-23 inhibitors have a sound preclinical basis for use in autoimmune hemolytic anemia and might open up a new steroid free option or allow early steroid withdrawal in hemolytic anemia.
The woman was treated at the hospital for shortness of breath and chest pain that had lasted for a few weeks. She was found to have low blood hemoglobin levels, a sign of anemia.
Doctors attributed the patient’s anemia to her history of long menstrual bleeds and liver disease. She was treated with red blood cell infusions — leading to an increase in hemoglobin levels — and was discharged.
Yet, she came back two weeks later with similar symptoms. Additional laboratory and clinical testing revealed a number of blood abnormalities consistent with an AIHA diagnosis. Among them were several markers of hemolysis, such as increased levels of lactate dehydrogenase (LDH) and undetectable haptoglobin levels.
Further testing showed the woman had red blood cell clumping, a hallmark of AIHA, and was positive for both cold agglutinins and warm self-reactive antibodies. These findings confirmed a diagnosis of mixed AIHA. The woman also showed evidence of immune complement system activity, a known contributor to AIHA.
Use of IL-23 inhibitor may allow early steroid withdrawal
Treatment included weekly into-the-vein (intravenous) rituximab infusions and prednisone, which was gradually tapered off. She showed improvements, but at a follow-up a year later, her anemia and signs of hemolysis had returned.
She was restarted on steroids and given another course of rituximab treatment. Again, she acutely improved but worsened eight months later. At this point, “multiple treatment options … were discussed,” the researchers wrote, but “based on patient preference, she received another course of rituximab.”
Again, her hemoglobin levels normalized after two months, but this time she showed no signs of disease relapse for up to two years.
Her case was then further analyzed, “given her interesting disease course and now sustained remission,” the researchers wrote.
The team found that the woman’s haptoglobin levels had normalized within the prior 14 months, although they had been undetectable or abnormal at every other point since her initial diagnosis.
A closer look at her medical records revealed that she had been started on risankizumab to treat her psoriasis at that point. Ultimately, the woman had become negative for cold agglutinins and exhibited no signs of hemolysis since she had started the IL-23 inhibitor.
Given their findings, the researchers “speculate the potential use of IL-23 inhibitors in treating AIHA,” they wrote, noting that such medications may have a better safety profile than long-term steroid use.
“Detailed preclinical analysis of IL-23 inhibitors in models of AIHA will further support this possibility,” the team concluded, adding, “IL-23 inhibitors have a sound preclinical basis for use in autoimmune hemolytic anemia and might open up a new steroid free option or allow early steroid withdrawal in hemolytic anemia.”