COVID-19 worsens CAD symptoms in 71-year-old man: Case report
Preexisting autoimmune diseases may be exacerbated by COVID-19
Written by |
Infection with SARS-CoV-2, the virus that causes COVID-19, worsened symptoms of cold agglutinin disease (CAD) in a 71-year-old man in whom the autoimmune disease had been stable, a U.S. study reports.
This case highlights the need for clinicians to be “mindful of potential preexisting … conditions, particularly [blood-related] diseases, that can be exacerbated by COVID-19,” researchers wrote.
The case report, “Acute Exacerbation of Cold Agglutinin Disease by SARS-CoV-2 Infection: A Rural U.S. Hospital Experience,” was published in the journal Annals of Internal Medicine Clinical Cases.
CAD is a type of autoimmune hemolytic anemia (AIHA), a group of rare autoimmune conditions marked by the production of self-reactive antibodies that wrongly target red blood cells, marking them for destruction in a process called hemolysis.
In CAD, self-reactive antibodies of the IgM class called cold agglutinins bind to red blood cells at low temperatures. Conversely, in warm AIHA, this process is driven by self-reactive antibodies of another class, IgG, that attack red blood cells at higher temperatures. Patients with both types of self-reactive antibodies are said to have mixed AIHA.
Worsening CAD symptoms have been linked to COVID-19
AIHA can occur secondary to infections, and a number of studies have reported new or worsening CAD symptoms following SARS-CoV-2 infection or after vaccination against COVID-19.
In the report, clinicians at White River Health, in Batesville, Arkansas, described the case of an elderly man with CAD whose symptoms worsened following SARS-CoV-2 infection.
The man was admitted to their hospital after experiencing weakness and lightheadedness for two days. Besides stable CAD, his medical history included heart failure, high levels of fatty molecules in the blood, and chronic lymphocytic leukemia, a type of blood cancer affecting certain immune cells and that develops slowly over time.
The patient was being monitored at another hospital, and his treatment included Imbruvica (ibrutinib), a leukemia therapy.
On physical examination, he was found apathetic, with a pale color in the lining of his eyes. Examination of his heart, lungs, and abdomen found no abnormalities.
Blood work showed below-normal levels of hemoglobin, which is the protein in red blood cells that carries oxygen, white blood cells, and platelets (tiny cell fragments involved in blood clotting).
Additionally, the man had signs of hemolysis, including low levels of the protein haptoglobin and elevated levels of the protein bilirubin and the enzyme lactate dehydrogenase.
In agreement with his CAD diagnosis, he was positive for cold agglutinins and tested positive on a direct Coombs test, which detects antibodies bound to red blood cells. The test came back negative for IgG antibodies, ruling out warm AIHA.
At this time, he also tested positive for SARS-CoV-2 infection, but didn’t require oxygen supplementation.
While rituximab (sold as Rituxan in the U.S., with biosimilars available) is commonly used off-label as a first-line treatment for CAD, the immunosuppressive therapy has been shown to worsen mortality for hospitalized COVID-19 patients with preexisting autoimmune diseases.
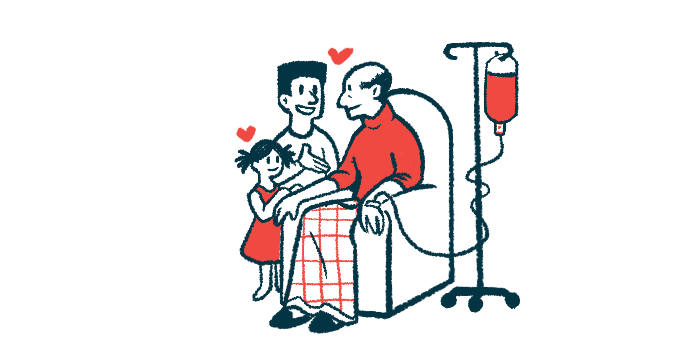
Patient treated with steroids, blood transfusions, folate supplementation
As such, the man was treated with steroids instead. Even though this type of anti-inflammatory and immunosuppressive medication rarely works in CAD, it was shown to reduce risk of death in certain COVID-19 patients.
“We chose to use steroids to help prevent further clinical worsening due to COVID-19,” the team wrote.
He also received blood transfusions and folate supplementation to help restore red blood cell counts.
The man responded well to treatment, with his hemoglobin levels increasing slightly, and he was discharged from the hospital. Rituximab treatment was scheduled to start two weeks after he recovered from COVID-19.
Overall, “this case report shows that preexisting cold agglutinin disease can be exacerbated by SARS-CoV-2 infection,” the clinicians wrote.
“The decision whether to use rituximab in patients with COVID-19 should consider risk and benefit, based on the severity of hemolysis, the patient’s underlying … conditions, and response to transfusion,” they concluded.