COVID-19 may trigger production of cold-reactive antibodies: Report
Japanese man treated for severe anemia tested positive for cold agglutinins
Written by |
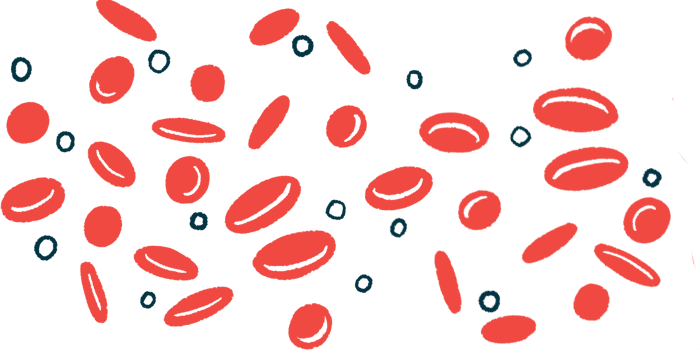
A Japanese man with severe anemia — a condition marked by too few red blood cells in the body — following a case of COVID-19 tested positive for cold agglutinins and cryoglobulins, two types of antibodies that become reactive in the cold, according to a new report.
Cold agglutinins are the cause of cold agglutinin disease, or CAD, and cryoglobulins characterize another rare condition called cryoglobulinemia.
While cold agglutinins can cause hemolysis, or the destruction of red blood cells, there were no longer signs of this by the time the patient was first tested for cold agglutinins, the report noted. Also, the man’s anemia was resolved with a blood transfusion and folic acid, a lab-made form of the vitamin folate, which helps the body make red blood cells.
However, two months later, the man still tested positive for cryoglobulins, even though he showed no symptoms of cryoglobulinemia, including thrombosis — blood clots that block blood flow.
This case suggests that COVID-19 may trigger the production of cold-reactive antibodies, but these may “not necessarily cause clinically significant hemolysis or thrombosis,” the researchers wrote.
As such, immunosuppressive treatment may not be necessary for all cases of cold-related blood disorders following COVID-19 infection, the team noted.
The case report, “Coexistence of Cold Agglutinin and Cryoglobulin in a Patient With Severe Anemia Following COVID-19 Infection,” was published in the journal Cureus.
Treatment sought after anemia worsened following COVID-19 diagnosis
CAD is a rare autoimmune disease marked by the production of self-reactive antibodies called cold agglutinins that bind to red blood cells at reduced temperatures, marking the cells for destruction. The disease can occur due to an unknown cause, or secondary to other conditions, such as infections.
A number of studies have reported CAD symptoms following infection with SARS-CoV-2, the virus that causes COVID-19.
One previous study reported that more than half of CAD patients also have cryoglobulins, which may change how symptoms manifest. Cryoglobulins are abnormal antibodies that become insoluble and clump together at reduced temperatures. This can block blood flow and cause blood vessels to become inflamed.
Cryoglobulinemia also is associated with other conditions, such as infections and autoimmune diseases, but there have been few reports of cryoglobulinemia linked to COVID-19.
Here, a team from the Uwajima City Hospital in Japan detailed the case of a 73-year-old man who was referred to their hospital due to worsening anemia following COVID-19.
The patient had been diagnosed with COVID-19 two months earlier. About three weeks after that diagnosis, blood testing revealed signs of hemolysis, with high levels of bilirubin and lactate dehydrogenase, and few and larger-than-normal red blood cells. Both bilirubin and lactate dehydrogenase are released into the bloodstream with hemolysis.
Hemoglobin — the protein in red blood cells that carries oxygen across the body — also was dropping over time. The man “was referred to our hospital 40 days after COVID-19 infection,” the researchers wrote.
High levels found of 2 types of antibodies that become reactive in cold
Further testing showed that the patient’s red blood cells appeared normal in size. However, there were few reticulocytes, or immature red blood cells, which suggested his body wasn’t making enough of them. Blood levels of hemolysis markers, including bilirubin and lactate dehydrogenase, were normalized, but the levels of folate were very low, the results showed.
The man also showed high levels of cold agglutinins and cryoglobulins, and his blood formed clumps at low temperatures. A direct Coombs test, which checks whether certain antibodies and complement proteins are attached to red blood cells, came back positive for the latter. Complement proteins are a part of the immune system that is known to contribute to CAD-related hemolysis.
The results confirmed a CAD diagnosis. Hemolysis associated with cold agglutinins “may have been present immediately after COVID-19 infection,” the team wrote. However, they noted that “the cause of subsequent anemia progression is difficult to explain by hemolysis.”
According to the researchers, the data highlighted that “not all patients with [viral] infections who develop secondary [CAD] will have clinically significant hemolysis.” But “we consider that the severe reduction in the red blood cell count in this case is likely multifactorial, with folate deficiency playing a significant role,” the team added.
The present case highlights the importance of understanding the underlying causes and consequences of cold-related [blood] disorders following COVID-19 infection, as well as choosing optimal medical interventions.
The man was given a blood transfusion and started on oral folic acid supplements. His condition improved steadily, per the report. Two months later, he showed no symptoms, his cold agglutinin levels were nearly normalized, and the result of the direct Coombs test became negative.
Although he still tested positive for cryoglobulins, he continued to show no symptoms of cryoglobulinemia, including thrombosis, the researchers noted.
While immunosuppressive treatments are often used for these diseases, “the present case highlights the importance of understanding the underlying causes and consequences of cold-related [blood] disorders following COVID-19 infection, as well as choosing optimal medical interventions,” the team wrote.
Because immunosuppressants like corticosteroids can have serious side effects, their use “should be considered carefully,” they concluded.