Antibody Modification May Drive Antibody-linked Diseases Like CAD
A type of protein modification called glycosylation is associated with higher levels of disease-causing antibodies in cold agglutinin disease (CAD), new research suggests.
The findings highlight the role that antibody modifications play in antibody-driven diseases like CAD, researchers said.
The study, “In from the cold: M‐protein light chain glycosylation is positively associated with cold agglutinin titer levels,” was published in Transfusion.
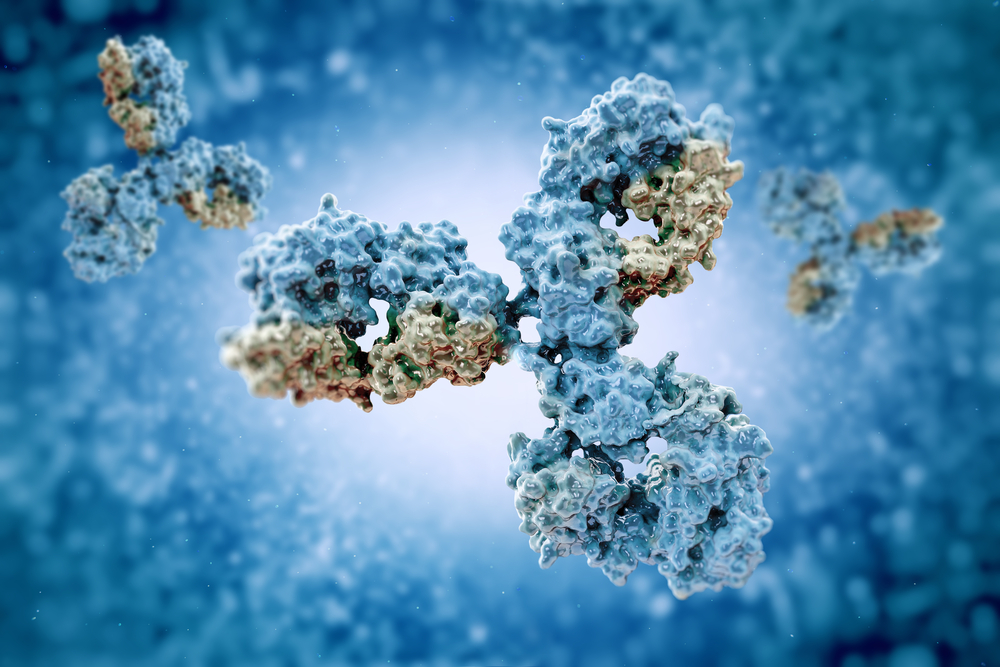
CAD is caused by antibodies called cold agglutinins, which bind to red blood cells at low temperatures, causing the cells to be destroyed. Cold agglutinins and other antibodies are complex proteins that undergo various biochemical modifications when they are produced.
One such change is glycosylation, in which sugar molecules are attached to the antibody. Recent research has demonstrated that antibodies with more glycosylation tend to last longer in the body, and may behave differently in other ways as well.
Researchers with the Mayo Clinic and the Medical College of Wisconsin wondered if cold agglutinin glycosylation was involved in the development of CAD.
To test this idea, the researchers used biochemical assays to examine antibody glycosylation using blood samples from 77 people, including 21 with a clinical diagnosis of CAD. They also analyzed 48 patient samples from a reference laboratory, with varying cold agglutinin levels and unclear CAD status.
Overall, the researchers found that higher antibody glycosylation was associated with higher levels of cold agglutinins, as well as higher levels of monoclonal antibodies in general. Monoclonal antibodies, also called M-proteins, are antibodies that are structurally identical to one another and bind the exact same region in a molecule. Cold agglutinins are a form of monoclonal antibodies.
“Among those tested for CA [cold agglutinin] titers with M-proteins, patients with M-protein [glycosylation] were more likely to have a clinical diagnosis of CAD,” the researchers wrote.
The team also conducted analyses to examine whether antibody glycosylation was associated with differences in hemolysis (red blood cell destruction) in a laboratory setting. No statistically significant differences were detected.
“Further studies into the mechanistic role of M-protein [glycosylation] in the pathogenesis [disease development] of CAD are needed,” the researchers wrote.
More broadly, the team said that these findings, “align with the emerging body of research demonstrating that specific antibody modifications can have a role in antibody-mediated disease processes.”