CAD and Anesthesia
Written by |
For cold agglutinin disease (CAD) patients who may need to undergo surgery, certain complications can occur as a result of anesthesia, but there are some simple precautions that can be taken to lower the risk of these issues.
What is anesthesia?
Anesthesia involves the use of medications during medical procedures to prevent or manage pain. There are four main types of anesthesia: general, regional, and local anesthesia, and sedation.
General anesthesia renders patients unconscious and unresponsive to pain. Doctors usually administer it intravenously (IV) or through inhalation of gases. They continuously monitor patients for changes in heart rate, blood pressure, oxygen levels, and breathing.
Doctors use regional anesthesia to prevent pain signals in large regions of the body such as the lower body or a limb. They inject nerve-blocking medications into the spine or a peripheral nerve to achieve this type of anesthesia. Patients are usually still conscious during this time.
In local anesthesia, doctors administer medications to small areas of the body. Local anesthetics are usually in the form of injections, sprays, or ointments.
Doctors often use sedation for minor surgeries. These can range in strength from leaving patients drowsy to not being able to remember the surgery. Painkillers may also be necessary.
When might a CAD patient need anesthesia?
CAD may increase the risk of heart problems and the need for heart surgery. CAD can also affect the liver and spleen and cause problems that may require surgery and anesthesia.
Possible CAD-related complications
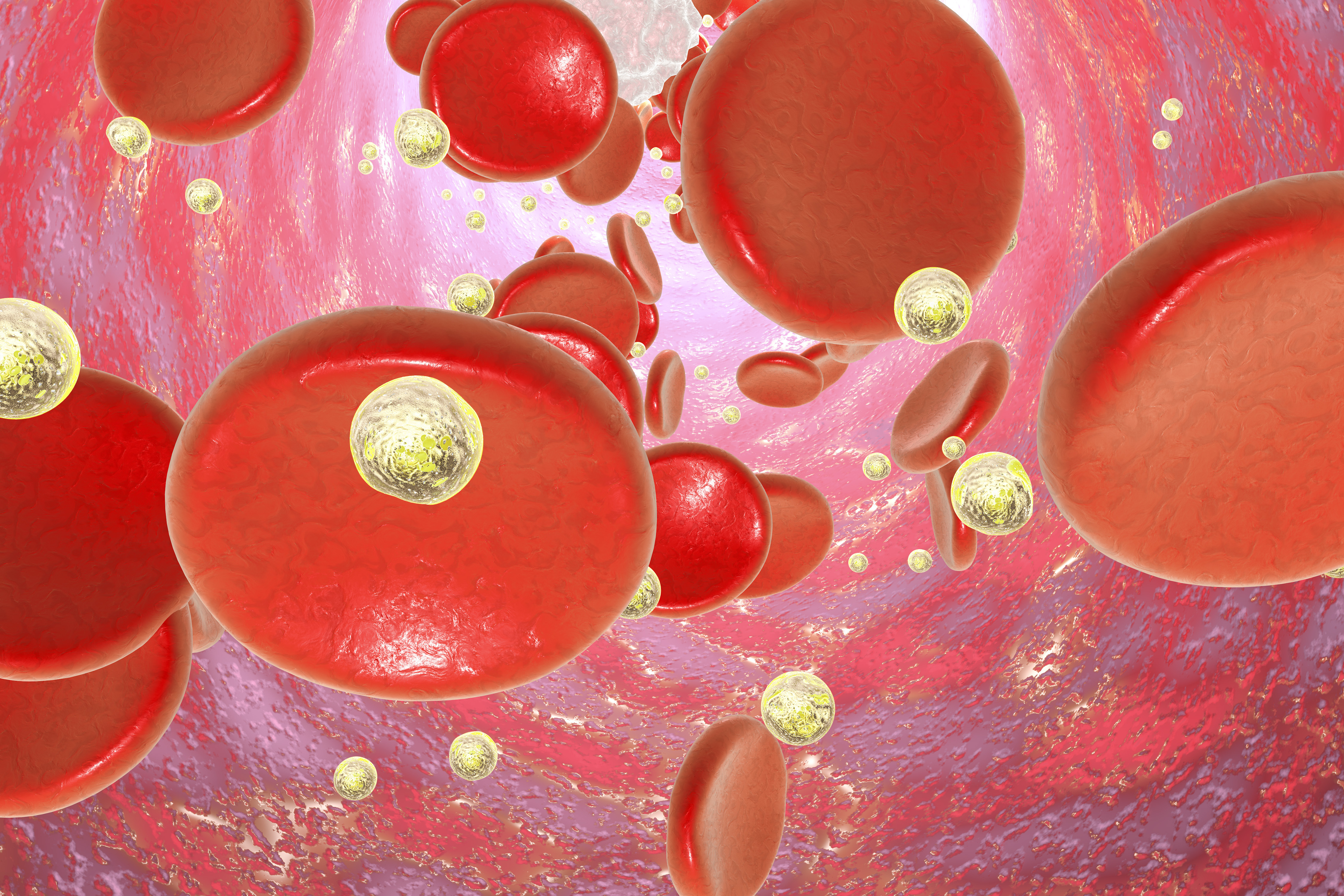
During anesthesia, patients may receive treatment through injections, infusions, or gases they inhale. Many medications are refrigerated to preserve them before use. If doctors give them to CAD patients cold, this can result in the activation of cold agglutinins, autoantibodies that mistakenly bind to red blood cells at low temperatures. Most gases are stored compressed in cylinders, and when they are released and expand, this causes them to cool. When the cool gases reach the blood in the lungs, it can also lead to activation of the cold agglutinins and complications.
What precautions should doctors take?
There are several simple strategies doctors can follow to lower the risks associated with CAD during medical procedures. For example, they should ensure all fluids and gases they are using for anesthesia are as close to body temperature as possible. They can increase the temperature of fluids using blood warmers. They can also warm and humidity gases using a heat and moisture exchanger.
Doctors may also use plasma exchange during anesthesia to replace the patient’s plasma (the clear fluid of the blood) that contains cold agglutinins with artificial plasma without the autoantibodies or a mixture of many different antibodies to reduce the risk of clots. The plasma should be warm as well.
Doctors should also monitor patients’ internal and peripheral body temperatures during any surgical procedures. It is important to make the room temperature as warm as possible and as tolerable for the medical staff. Warming blankets that cover all non-procedural areas of the body can also keep the patient from getting too cold.
Last updated: Dec. 10, 2020
***
Cold Agglutinin Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.