Enjaymo (sutimlimab-jome) for cold agglutinin disease
Last updated Nov. 7, 2024, by Marta Figueiredo, PhD

What is Enjaymo for cold agglutinin disease?
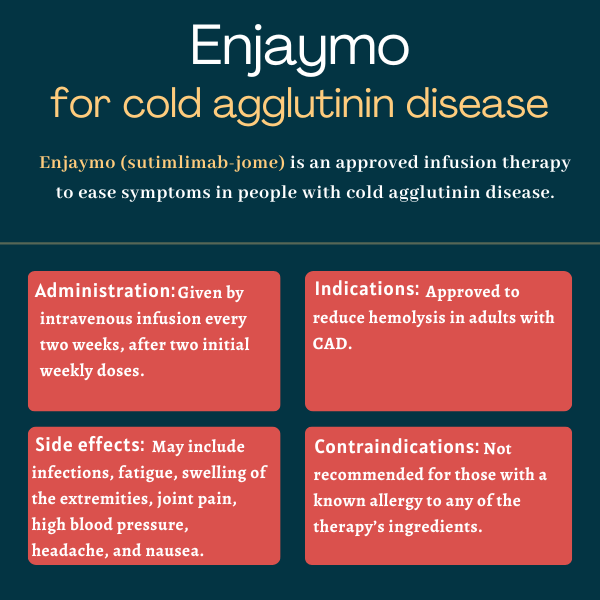
Enjaymo (sutimlimab-jome) is an infusion therapy approved to reduce hemolysis, or red blood cell destruction, in adults with cold agglutinin disease (CAD).
The medication, which is the only approved treatment for CAD, is designed to ease disease symptoms and improve quality of life. It is administered via an intravenous, or into-the-vein, infusion every two weeks.
Enjaymo was initially developed by Bioverativ, which was acquired by Sanofi in 2018. Sanofi continued to develop the treatment until 2024, when it sold the global rights to Enjaymo to Recordati.
Therapy snapshot
| Brand name: | Enjaymo |
| Chemical name: | Sutimlimab-jome |
| Usage: | Used to treat hemolysis in adults with CAD; can reduce disease symptoms |
| Administration: | Intravenous infusion |
How does Enjaymo work?
CAD is a rare autoimmune disorder in which self-reactive antibodies called cold agglutinins mistakenly attack red blood cells at cold temperatures, tagging them for destruction (hemolysis).
This can result in anemia, which is defined as fewer-than-normal red blood cells or low levels of hemoglobin, the protein in red blood cells that transport oxygen throughout the body. Hemolysis and anemia are responsible for most CAD symptoms.
When cold agglutinins bind to their target, they activate a part of the immune system called the complement system. This is a set of more than 30 proteins that are normally found in circulation in an inactive state. However, in response to certain stimuli, such as an infection or the autoantibodies that drive CAD, the complement system becomes activated, with proteins triggering each other in a cascade.
In CAD, hemolysis is particularly dependent on the activation of the classical complement pathway, one of the three pathways that make up the complement system.
Enjaymo, previously known as BIVV009 or TNT009, is an antibody-based therapy that works by selectively blocking the complement C1s protein, which is responsible for starting the classical complement cascade. By suppressing this pathway, the therapy can reduce hemolysis and increase hemoglobin levels, which is expected to ease CAD symptoms, reduce or eliminate the need for blood transfusions, and improve quality of life.
Also, the fact that Enjaymo targets only one complement pathway ensures the complement system is not completely blocked. A complete inhibition could significantly limit patients’ ability to fight microbes and other threats.
Who can take Enjaymo?
Enjaymo was approved by the U.S. Food and Drug Administration in February 2022 to reduce the need for blood transfusions due to hemolysis in adults with CAD. It became the first therapy approved for this rare condition.
About a year later, Enjaymo’s indication was updated in the U.S. to include its use to reduce hemolysis in adult CAD patients regardless of their history of blood transfusions.
In November 2022, the therapy was approved in Europe for hemolytic anemia, or anemia due to hemolysis, in adults with CAD.
Who should not take Enjaymo?
According to its prescribing information, Enjaymo should not be used by anyone with a known allergy to any of its ingredients.
How is Enjaymo administered?
Enjaymo is administered by a healthcare provider as an infusion directly into the bloodstream. The recommended dose is based on the patient’s body weight:
- 6,500 mg, for those weighing 39 kg to less than 75 kg (about 86-165 pounds)
- 7,500 mg, for those weighing 75 kg (165 pounds) or more.
The medication is available in single-dose vials containing 1,100 mg of the therapy’s active ingredient in 22 mL of a solution that’s clear to slightly milky, or colorless to slightly yellow.
Injections should be given once weekly for the first two weeks, and every other week thereafter, with flexibility to administer each dose within two days of the scheduled timepoints. The infusion period depends on the patient’s body weight and the presence or absence of cardiopulmonary disease, but it usually takes place over one to two hours.
If a scheduled Enjaymo dose is missed, an infusion should be given as soon as possible, and dosing every two weeks should resume from that point on. However, if there’s a delay of more than 17 days, the next two doses should be given with a one-week interval before resuming every-other-week administration.
Enjaymo in clinical trials
Enjaymo’s approvals were based primarily on data from a pair of global Phase 3 clinical trials, dubbed CARDINAL (NCT03347396) and CADENZA (NCT03347422).
CARDINAL
The two-part CARDINAL study evaluated the safety and effectiveness of Enjaymo in 24 adults with primary CAD who received at least one blood transfusion within six months of enrolling.
In part A of the study, all participants received the therapy for 26 weeks (about six months). The main goal was to assess whether Enjaymo could increase hemoglobin levels by at least 2 grams per deciliter (g/dL), or normalize those levels to at least 12 g/dL, without the need for additional blood transfusions or other CAD medications after week five.
Results showed 54% of patients met this goal. When each measure was examined separately, 62% of patients achieved the target 2 mg/dL increase in hemoglobin levels, and 71% remained free from transfusions after week five. Also, 92% of patients were off of other CAD treatments.
Participants also experienced drops in mean blood levels of hemolysis markers (bilirubin and lactate dehydrogenase, or LDH) and clinically meaningful reductions in fatigue, as measured with the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue Scale, as early as one week of starting treatment. All these therapeutic benefits coincided with the nearly complete suppression of the classic complement pathway from week one onward.
Enjaymo treatment was also associated with sustained reductions in symptoms and quality-of-life improvements, as assessed via patient-reported measures, as well as substantial reductions in patient hospitalizations and blood transfusions.
After completing part A, participants continued to receive Enjaymo for up to two more years in an extension portion (part B). Longer-term treatment was associated with sustained benefits in hemoglobin and bilirubin levels, and patients also maintained their fatigue reductions and quality-of-life improvements through the 2.5 years of treatment.
However, among the 20 patients who completed part B and were followed for nine more weeks after stopping treatment, signs and symptoms of hemolysis had returned.
CADENZA
The two-part CADENZA study enrolled 42 adults with primary CAD and no recent blood transfusions, who were randomly assigned to receive either Enjaymo or a placebo for six months (part A). After that, all participants received the therapy for an additional year (part B).
The main goal in part A was to assess the percentage of patients experiencing a hemoglobin level increase of at least 1.5 g/dL without the need for blood transfusions or other CAD treatments from week five onward.
Data showed a significantly greater proportion of Enjaymo-treated patients achieved that outcome than those on the placebo (72.7% vs. 15%).
The therapy was also superior to the placebo at increasing hemoglobin levels, reducing bilirubin and LDH levels, and lessening fatigue, as assessed with the FACIT-Fatigue Scale. It also led to greater improvements in quality of life and reductions in symptoms of anemia.
Results from part B showed long-term Enjaymo treatment led to sustained reductions in hemolysis, anemia, and fatigue, as well as to life-quality improvements.
For those initially on the therapy, benefits observed in part A were generally maintained through part B. Those originally assigned a placebo also experienced similar benefits shortly after switching to Enjaymo in part B.
Similar to what was observed in CARDINAL, after a nine-week period without treatment, most benefits were reversed, with levels of blood markers and scores on patient-reported measures returning to those reported before participants started on Enjaymo.
Common side effects of Enjaymo
The most common side effects associated with Enjaymo include:
- high blood pressure
- urinary tract infection
- respiratory tract infection
- bacterial infection
- swelling in the lower legs or hands
- joint pain
- headache
- nausea
- rhinitis, or runny nose
- acrocyanosis, or bluish skin color in the hands, feet, and sometimes face
- dizziness
- fatigue
- cough
- Raynaud’s phenomenon, or changes in color or sensation in the fingers and toes due to blood vessels narrowing under cold or stressful conditions.
Infections
Enjaymo may increase a person’s susceptibility to serious infections, including those caused by encapsulated bacteria. These bacteria include Neisseria meningitides, which causes a form of meningitis; Streptococcus pneumoniae, associated with pneumonia; and Haemophilus influenzae, which can cause a range of severe infections.
For this reason, patients should be vaccinated against encapsulated bacteria at least two weeks before their first dose of Enjaymo, according to current vaccination guidelines for patients on complement-blocking therapies. If there is an urgent need to start Enjaymo treatment in patients not up to date on such vaccines, vaccination should be given as soon as possible.
Still, such vaccines do not completely eliminate the risk of encapsulated bacterial infections, so patients should be routinely monitored for early signs of serious infections. These signs may include fever, rash, chest pain, breathlessness, high heart rate, nausea, and headache. If an infection is suspected, patients should be immediately evaluated.
Patients with active whole-body infections while on Enjaymo should also be closely monitored for signs of worsening infection. The therapy may be interrupted in patients receiving treatment for a serious infection.
Infusion-related reactions
Enjaymo can cause infusion-related reactions, including allergic reactions that may be serious and life-threatening. In Phase 3 trials, infusion-related reactions, including shortness of breath, rapid heartbeat, nausea, headache, and low blood pressure, were reported in 29% of patients on Enjaymo. These reactions led to one patient discontinuing treatment.
If these reactions are detected, Enjaymo infusions should be slowed or interrupted altogether. If patients show signs of an allergic reaction, such as cardiovascular or respiratory problems, the therapy should be discontinued and appropriate supportive measures should be given as needed.
The treatment is not recommended for patients with known allergies to its active substance or its other ingredients.
Autoimmune diseases
Enjaymo may increase a person’s risk of developing autoimmune diseases, such as systemic lupus erythematosus. For this reason, those taking Enjaymo should be monitored regularly for signs or symptoms of an autoimmune condition and treated accordingly.
Hemolysis
If treatment with Enjaymo is interrupted, patients should be monitored closely for any signs or symptoms of hemolysis, including increases in blood markers of hemolysis, fatigue, shortness of breath, and the presence of blood in urine. Physicians may consider restarting Enjaymo if these signs happen after treatment is discontinued.
Use in pregnancy and breastfeeding
No data are available on the use of Enjaymo in people who are pregnant or breastfeeding, or on the presence of the medication in human milk and its effects on milk production. In animal studies, the use of Enjaymo during pregnancy at doses higher than those used in people did not cause any noteworthy problems in the mothers or their offspring.
Patients who are pregnant or nursing, or plan to become pregnant or breastfeed, should discuss this topic with their healthcare team, carefully weighing the potential risks and benefits of continuing or stopping treatment.
Cold Agglutinin Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- FDA fast-tracks potential new option for autoimmune blood diseases
- Long-term Enjaymo use shows favorable outcomes in CAD: Study
- With my health from CAD steadily declining, I call in the cavalry, part 1
- Genetic variations in underlying lymphoma influence AIHA types
- Lessons from ‘Winnie-the-Pooh’ help me navigate life with CAD
- Cost-effective rituximab-based treatment keeps CAD at bay for years
- This year, ongoing CAD symptoms dampened my holiday cheer
- Immunochemotherapy can help control CAD but it carries safety risks
- Oral therapy iptacopan eases anemia in CAD patients: Small trial
- When living with CAD, even a short trip can be a nightmare