Study Urges Careful Analysis of MAIHA Patients to Optimize Treatment
The profile of patients with mixed autoimmune hemolytic anemia (MAIHA) must be carefully analyzed to facilitate diagnosis and disease management, a study says.
The findings of the study, “Immunohematological and clinical characterizations of mixed autoimmune hemolytic anemia,” were published in the Asian Journal of Transfusion Science.
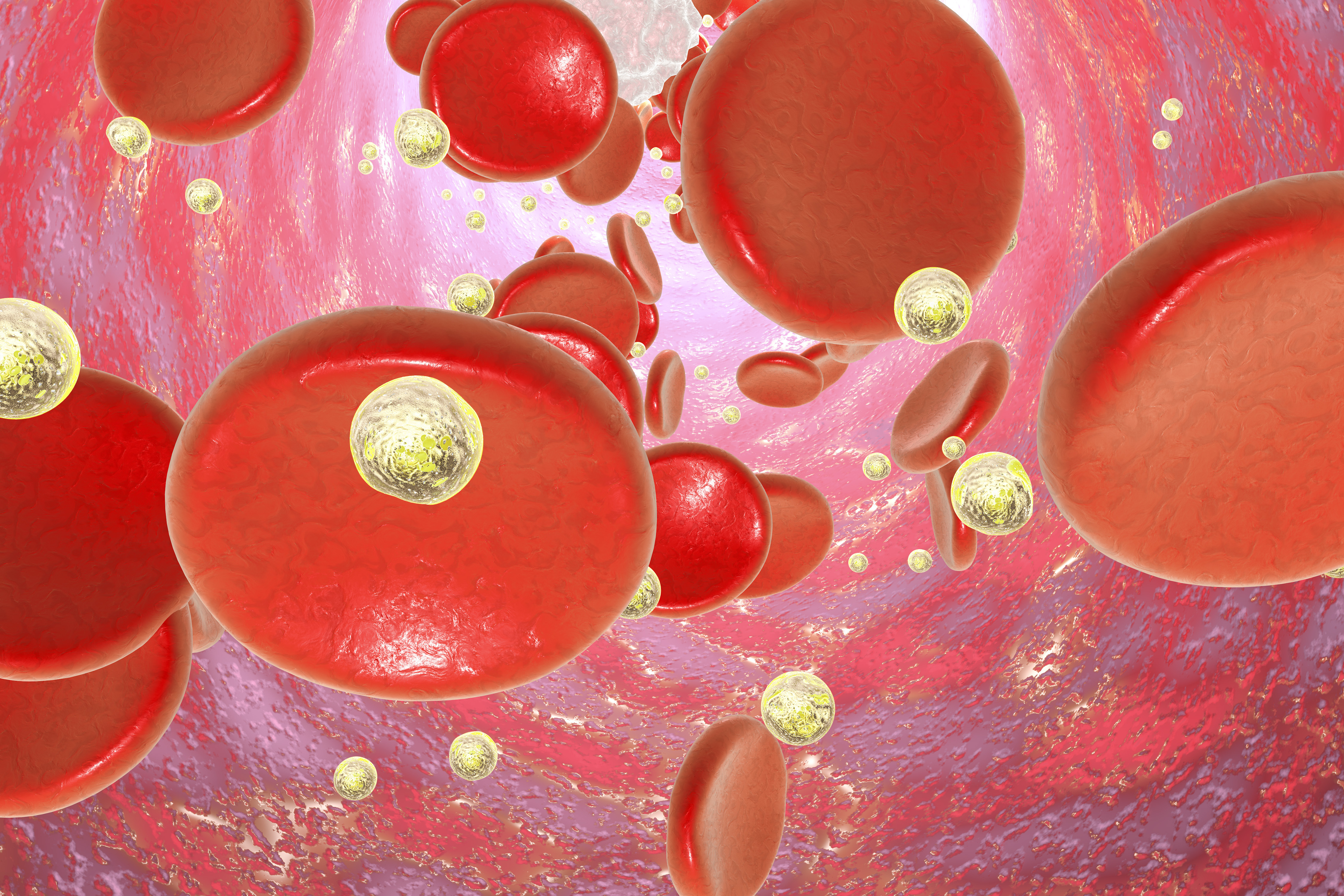
Autoimmune hemolytic anemia (AIHA) is characterized by the production of autoantibodies that attack and destroy red blood cells. It includes three variants — cold agglutinin disease (CAD), warm autoimmune hemolytic anemia (wAIHA) and MAIHA — depending on whether autoantibodies’ binding to red blood cells is easier at lower, higher or both low and high temperatures.
“Patients with MAIHA have a chronic [disease] course interrupted by severe exacerbations, which can result in severe anemia at times. [For this reason, patients] may need blood transfusion and blood units have to be released as ‘best match’ units due to serological incompatibility caused by the [presence of different types of] autoantibodies,” the researchers said.
In this study, a team of Indian researchers performed a deep characterization of the immunologic and hematologic (blood-related) profiles of patients with MAIHA.
The study, carried out between July 2013 and August 2017, involved 217 patients suspected of having AIHA. Of these, 134 patients received a positive diagnosis of AIHA — 89 (66.4%) with wAIHA, 32 (23.9%) with CAD and 13 (9.7%) with MAIHA — based on clinical and antibody-serum analysis.
Among the MAIHA patients, eight had severe hemolysis (red blood cells’ destruction) and most were severely anemic and weak , requiring urgent blood transfusion.
As expected, lab analysis showed that all MAIHA patients’ samples contained multiple types of autoantibodies bound to their red blood cells. Blood group discrepancies were found in four (30.8%) patients. Based on this information, clinicians performed 29 blood transfusions with “best match” units of packed red blood cells in 12 out of the 13 MAIHA patients.
At follow-up, nine (69.2%) patients who received blood transfusions had significant improvements in immunologic and hematologic parameters. No adverse reaction to treatment was found in any of the study participants.
“We conclude that detailed clinical and immunohematological (immune and blood) characterization is needed to diagnose and manage MAIHA. Whereas corticosteroid and immunosuppressant therapies are the primary therapy … no critical patient should be denied blood transfusion due to serological complications,” the investigators concluded.