Stem cell transplant for lymphoma successful for man with severe CAD
Procedure can be done safely in CAD patients if precautions are taken: Report
Written by |
An autologous stem cell transplant (ASCT) to treat lymphoma, a blood cancer, was safely performed in a man with severe cold agglutinin disease (CAD) who was dependent on blood transfusions, researchers in Canada have reported.
Several strategies for a successful transplant were used to avoid potential complications from CAD. The strategies included several sessions of plasma exchange before stem cell collection, therapy to block the complement pathway, careful temperature control, and close teamwork among medical specialists.
Plasma exchange is a blood-cleaning procedure that can be used in CAD to remove the self-reactive antibodies that drive the autoimmune disease. The complement pathway is a part of the immune system that is involved in CAD-related abnormal immune reactions.
“This is the first case of successful ASCT in a patient with severe, transfusion-dependent CAD,” researchers wrote.
The case study, “Approach to autologous stem cell transplantation in a patient with severe cold agglutinin disease, a case report,” was published in Transfusion.
CAD is a rare autoimmune disease caused by the immune system’s abnormal production of self-reactive antibodies, called cold agglutinins, that bind to red blood cells at low temperatures. This causes red blood cells to clump together, activating the complement cascade that marks the cells for destruction in a process known as hemolysis. Symptoms like anemia, when the number of red blood cells is too low, and fatigue can result.
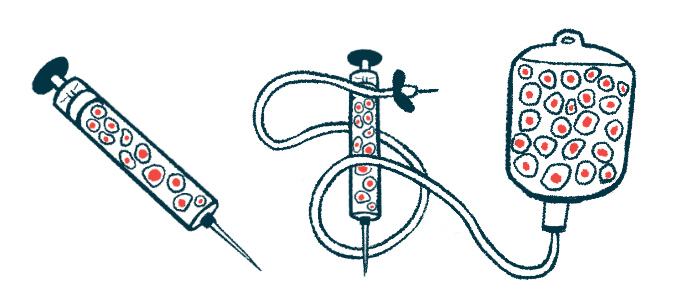
Autologous stem cell transplant used to treat blood cancers
An autologous stem cell transplant, commonly used to treat blood cancers, first involves the collection of healthy blood stem cells, which can give rise to all types of blood cells, from a patient. After chemotherapy or radiation therapy to kill the cancerous cells, the cells are infused back into the patient to replenish the body with new healthy blood cells.
As the procedure involves “several procedures that are performed at lower than body temperatures,” the researchers wrote, stem cell transplants in people with CAD “is particularly challenging” as it can trigger red blood cell clumping and hemolysis.
Now, a team of researchers in Canada described the case of a 61-year-old man with severe CAD who safely underwent ASCT for relapsing lymphoma.
The man developed symptoms of CAD in 2008. Several tests confirmed high levels of cold agglutinins and the presence of complement proteins bound to red blood cells, confirming a CAD diagnosis.
While CAD can also occur secondary to blood cancers, there was no evidence of blood cancer at that time. Immunosuppressive treatment with rituximab, cyclophosphamide, vincristine, and prednisone eased the patient’s symptoms, but he still needed regular blood transfusions.
In 2016, the man was diagnosed with a type of lymphoma that affects B-cells, the immune cells that produce antibodies, and also showed signs of increased hemolysis. Cancer treatment helped him reach complete disease remission, but he remained transfusion-dependent.
Patient started on Enjaymo
Two years later, the man was started on Enjaymo (sutimlimab-jome), a complement-blocking therapy approved for CAD, allowing him to become independent of blood transfusions.
His lymphoma relapsed some years later, and he was referred to the researchers’ center to undergo ASCT. Laboratory results showed continuous hemolysis and high cold agglutinin levels.
“We devised a strategy that hinged on patient optimization with [plasma exchange] and complement blockade, multimodal temperature control for all critical steps, and antibody/plasma depletion of the [transplanted stem cells],” the team wrote. Plasma is the liquid portion of blood that contains antibodies and complement proteins.
To remove cold agglutinins from the man’s blood and reduce the risk of red blood cell clumping, the patient underwent five plasma exchange sessions at warm temperatures before stem cell collection. He was also on maintenance therapy with Enjaymo.
The medical team carefully controlled temperatures in the room, bloodlines, solutions, and equipment to prevent complications during stem cell collection, handling, and re-infusion.
An infusion test, done a month before the full transplant, showed no red blood cell clumping, and later, the man successfully underwent the full transplant.
The experience gained from this case may also be applicable to other cell therapy procedures.
Man remained transfusion-dependent for 6 months after stem cell transplant
During recovery, he experienced a severe drop in hemoglobin, the protein in red blood cells that transports oxygen, due to hemolysis that required several blood transfusions. Despite continuing on Enjaymo, the man remained transfusion-dependent for the first six months after ASCT, but experienced some symptom relief.
A year after ASCT, the man still showed signs of hemolysis, but was free from blood transfusions. His lymphoma remained in remission.
The team noted that this was a more severe CAD case than the three other CAD cases undergoing ASCT that were previously reported. Also, CAD was secondary to the blood cancer in all other cases, “with resolution expected following lymphoma therapies,” while in this case, there was a need for “aggressive transfusion support” after the procedure.
This case shows that stem cell transplants can be done safely despite CAD if careful precautions are taken.
“The experience gained from this case may also be applicable to other cell therapy procedures,” the researchers concluded.