Rituximab for CAD does not raise risk of severe COVID-19: Study
However, patients with underlying autoimmune conditions may be at higher risk
Written by |
Rituximab does not seem to increase the risk for severe outcomes compared with other cold agglutinin disease (CAD) treatments in people who have the disease and COVID-19, according to a review study.
“Nonetheless, caution is advised when using rituximab in CAD patients with COVID-19 and underlying [autoimmune] conditions due to the heightened risk of severe outcomes in this subgroup, as reported in the literature,” researchers wrote.
The review, “Cold Agglutinin Disease and COVID-19: A Scoping Review of Treatments and Outcomes,” was published in the Journal of Clinical Medicine Research.
CAD is caused by a specific type of self-reactive antibodies, called cold agglutinins, that bind to red blood cells at cold temperatures, causing them to clump and be marked for destruction. This often results in tissues not receiving enough oxygen, which can lead to symptoms such as fatigue and pain.
Secondary CAD due to underlying cancer, autoimmune disease, infection
CAD is said to be primary when its cause is unknown, or secondary when it occurs due to an underlying condition, such as a blood cancer, another autoimmune disease, or an infection — including with SARS-CoV-2, the virus that causes COVID-19.
The current first-line treatment for CAD involves rituximab (sold as Rituxan, among others), an antibody-based therapy designed to target B-cells, the immune cells that produce antibodies, including cold-agglutinins.
However, “reports suggest that patients with both acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and cold agglutinin disease (CAD) may experience poorer survival when treated with rituximab,” the researchers wrote.
These observations were made among patients with underlying autoimmune conditions, which are usually treated with medications that suppress the immune system.
It is unclear whether the underlying autoimmune disease, marked by a more inflammatory state, or the use of other immunosuppressants — and not specifically rituximab — contributed to the reported worse outcomes.
To better understand rituximab’s effects in people with CAD and COVID-19, but no underlying autoimmune disease, a team of researchers in the U.S. systematically reviewed studies published up to December 2023 that reported disease outcomes in such cases.
The analysis included a total of 19 studies, 17 of them case reports and two were case series. Most were conducted in the U.S. (42%) and India (15%), and others across Europe and Asia.
We did not find an increased risk of severe outcomes among patients with CAD infected with COVID-19 who were treated with rituximab compared to those treated with other therapies.
Review included 23 patients with CAD and COVID-19
A total of 23 patients, mostly women (61%), with a mean age of 61 years, were included in the review. Most patients were diagnosed with CAD upon SARS-CoV-2 infection, with two patients previously diagnosed.
The most common initial symptoms were anemia, which means low levels of hemoglobin, or the protein in red blood cells that carries oxygen through the body, and severe pneumonia, a type of lung infection.
Patients often had other simultaneous health conditions, including high blood pressure, type 2 diabetes, kidney failure, cirrhosis (when the liver is severely scarred), chronic obstructive pulmonary disease, or leukemia (a type of blood cancer).
Treatments for CAD included rituximab, red blood cell transfusions, plasma exchange (a procedure that helps remove cold agglutinins), and immunosuppressive steroids, usually in combination. Rituximab was used in four patients (17.4%).
No significant difference was reported in the prevalence of co-existing health diseases between patients treated with rituximab and those given other therapies.
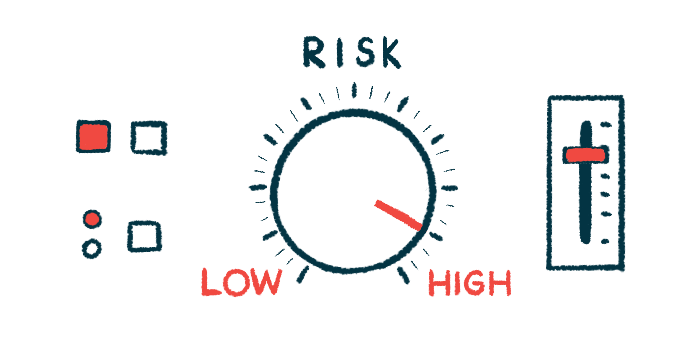
Overall, 17 patients (74%) recovered, while five (21%) died. No outcomes were reported for one patient. Nine patients (39%) were admitted to an intensive care unit (ICU).
More deaths reported for patients on treatments other than rituximab
Among patients treated with rituximab, one (25%) was admitted to the ICU, and none died. In contrast, among the 19 patients who received other treatments, eight (42%) were admitted to the ICU, and five (26%) died.
“We did not find an increased risk of severe outcomes among patients with CAD infected with COVID-19 who were treated with rituximab compared to those treated with other therapies,” the researchers wrote, adding, however, that the findings were based on case reports and case series alone.
In previous reports, the simultaneous use of other immunosuppressants in people with underlying autoimmune conditions may have erroneously attributed the increased risk of severe outcomes to rituximab therapy, the team noted.
“There is a need for further studies examining the effect of rituximab use among COVID-19 patients with CAD and [autoimmune] conditions while adjusting for underlying immune suppression of these autoimmune conditions,” the researchers concluded.