Lower C3, C4 Complement Proteins Levels Found in CAD Patients
Written by |
People with cold agglutinin disease (CAD) have significantly lower blood levels of C3 and C4 — two key molecules of the body’s innate complement immune system — than their healthy peers, a study found.
Notably, CAD patients showed the lowest levels of C3 and C4 among autoimmune hemolytic anemias (AIHAs), a group of rare disorders.
These findings may help scientists to better understand the underlying mechanisms of these diseases, and to improve diagnosis and treatment, the researchers said.
The study, “Features of serum complement C3 and C4 levels in autoimmune hemolytic anemia patients,” was published in the International Journal of Laboratory Hematology.
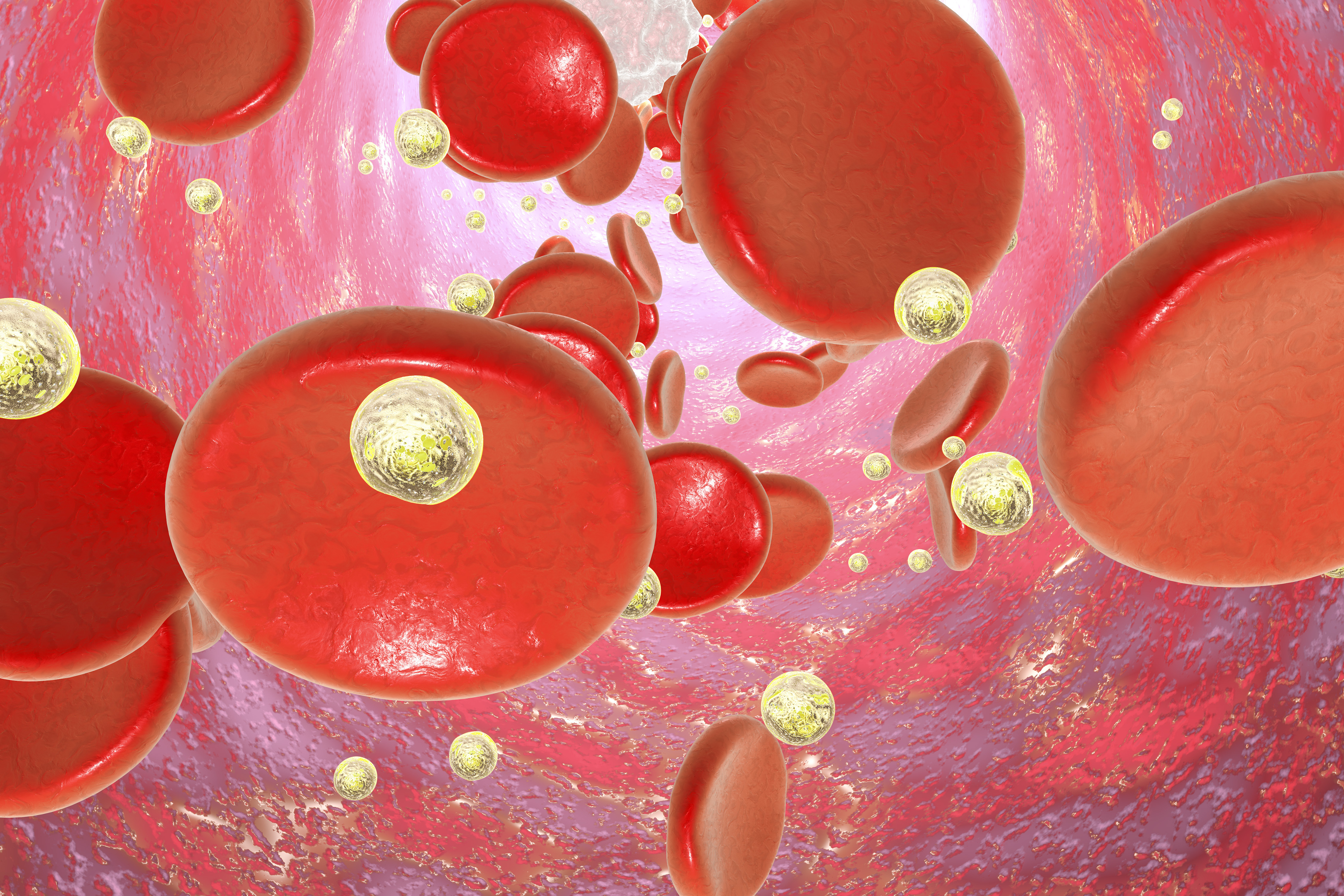
AIHA is a group of rare autoimmune diseases in which the immune system abnormally produces autoantibodies — immune proteins that mistakenly target a person’s own tissues or organs — against red blood cells, leading to their destruction (hemolysis).
It can be classified as CAD, warm AIHA (wAIHA), and mixed AIHA, depending on whether these autoantibodies bind more easily to red blood cells at lower or higher temperatures. The mixed type has both forms of antibodies.
Hemolysis in CAD and wAIHA is mediated by different mechanisms. In CAD, red blood cell destruction is dependent on the activation of the classical complement pathway. Meanwhile, that process is mainly driven by certain immune cells in wAIHA, although complement activation also may occur in some cases.
The complement system is a set of more than 30 blood proteins, mainly produced by the liver, that contribute to the body’s natural immune defenses.
Cold agglutinins, the autoantibodies produced in CAD, can be detected using the cold agglutinin test, whereas the warm-reaction autoantibodies and complement proteins are detected with the direct antiglobulin test (DAT). DAT-positive patients are those who tested positive for C3d, a complement protein, and/or IgG, an antibody; both are associated with hemolysis.
While abnormal activation of the complement system is involved as part of AIHAs, few studies have analyzed the levels of complement proteins in these patients.
Now, researchers in China have retrospectively analyzed the levels of two key complement proteins, C3 and C4, in the blood of 146 people with different AIHA subtypes and 110 healthy individuals (the control group).
Particularly, the study included 16 CAD patients — nine men and seven women, with a mean age of 58.5 (range, 18–72 years). In five of them, the disease was associated with other conditions (secondary CAD).
Other groups included 10 patients with DAT-negative, 74 DAT-positive primary wAIHA, 21 with DAT-positive wAIHA secondary to blood disorders characterized by uncontrolled production of certain immune cells, and 25 with DAT-positive wAIHA secondary to connective tissue disease.
The results showed that all groups of AIHA patients had significantly lower C3 and C4 levels in the blood compared with healthy individuals. The only exception was DAT-negative AIHA patients, who showed similar C4 levels relative to the control group.
Given that activation of either C3 and C4 leads to their degradation into components that activate the next protein in the complement pathway, low levels of these proteins are usually associated with activation of the complement system.
Notably, CAD patients, along with those with wAIHA secondary to connective tissue diseases, showed the lowest levels of both complement proteins, suggesting that complement activation may be more involved in these AIHA types, the team noted.
In addition, lower C4 levels were significantly associated with higher levels of cold agglutinins and C3d, but not of IgG. This reinforces that the C4 level drop in complement-mediated AIHA patients (CAD and some wAIHA) is due to complement activation and C4 breakdown.
Lower levels of both C3 and C4 also were linked to high levels of bilirubin, a biomarker of hemolysis. The researchers highlighted that patients with more severe hemolysis have lower C3/C4 levels “due to stronger activation of the complement system.”
Overall, these findings indicate that “complement levels in AIHA patients may be correlated with DAT patterns and underlying diseases,” the team added.
“These findings may be helpful in not only unraveling the mechanism underlying hemolysis in AIHA, but also diagnosing AIHA and selecting targeted treatment strategies,” the researchers concluded.