EBV Infection Can Cause Cold Agglutinin Disease, Even Without Symptoms of Infection, Case Study Suggests
Written by |
A case of hemolytic anemia and high bilirubin in blood may mean that infection with Epstein-Barr virus (EBV) — the most common one leading to mononucleosis — can cause cold agglutinin disease, even in the absence of typical symptoms of infection, a study suggests.
In such instances, treatment with corticosteroids can be safe and beneficial, researchers say.
The case study, “EBV-related Cold Agglutinin Disease Presenting With Conjugated Hyperbilirubinemia: A Pediatric Case Report and Mini Review,” was published in the Journal of Pediatric Hematology/Oncology.
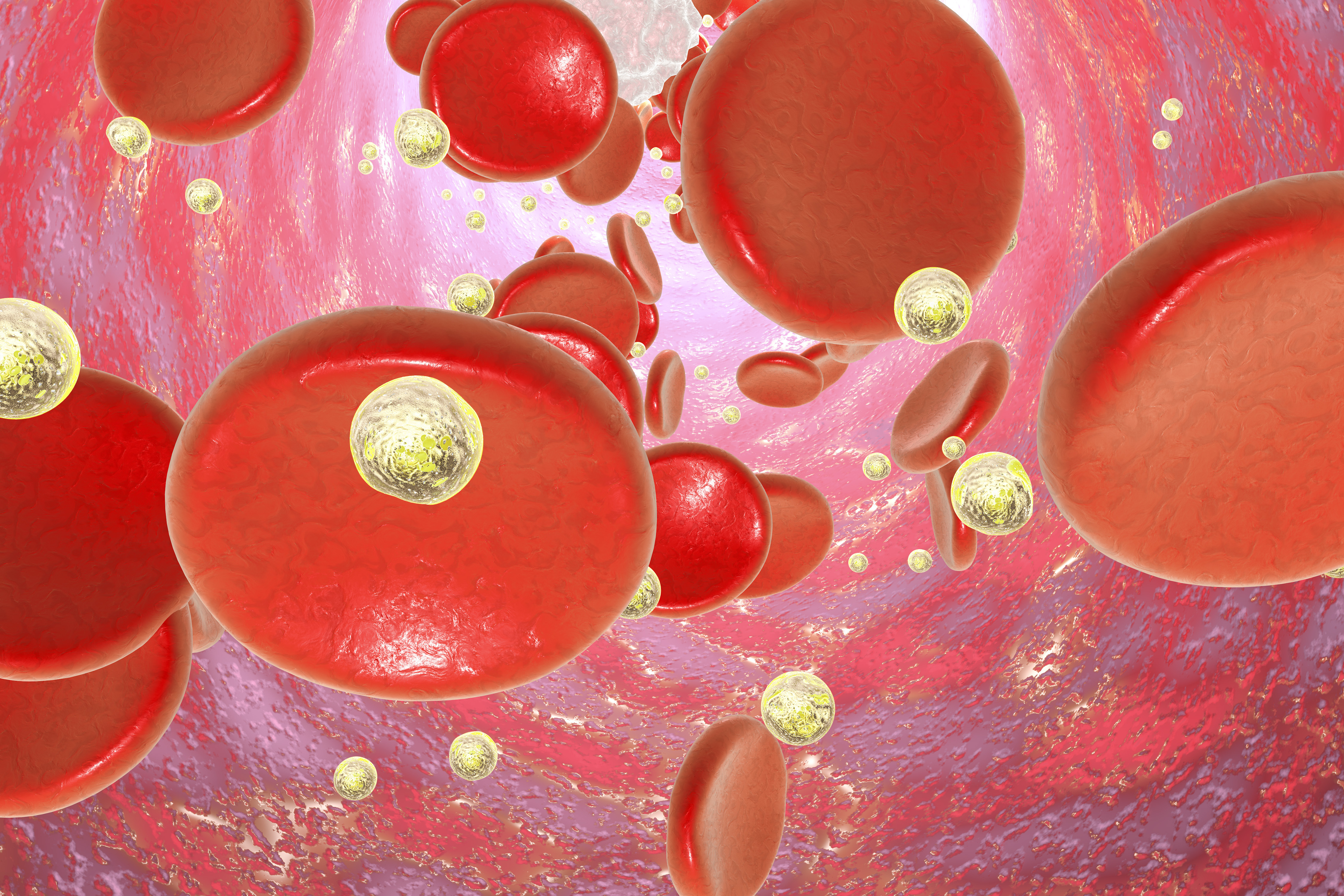
Cold agglutinin disease (CAD), or cold antibody hemolytic anemia, is a rare autoimmune disorder characterized by the abnormal destruction of red blood cells, which is caused by auto-antibodies attacking a person’s own cells.
What causes CAD is unknown, and it can appear as a disease by itself or be secondary to other disorders such as some infectious diseases that include mycoplasma infection, mumps, cytomegalovirus, or infectious mononucleosis, which is often caused by EBV.
Most people get infected with EBV at some point in their lives, usually during childhood. EBV infections in children normally do not cause symptoms, or the symptoms are not distinguishable from other mild childhood illnesses.
Teenagers and adults are more susceptible to complications such as infectious mononucleosis, also known as “mono” or “kissing disease.” The infection is typically mild and self-limited. However, in a few cases, people can develop hemolytic anemia, in which red blood cells are destroyed, resulting in low red blood cell counts.
In the study, physicians at the University General Hospital of Alexandroupolis, in Greece, described the case of a 8-year-old girl who entered the emergency room due to acute jaundice (yellow discoloration of skin and eyes due to high levels of bilirubin in her blood) and increasing fatigue, which had started five days prior, with accompanying fever and one episode of vomiting. She was hospitalized, and blood tests revealed she had low red blood cell counts (anemia).
Jaundice is caused by excess levels of bilirubin — a yellow-orange bile pigment produced during the liver’s normal process of breaking down red blood cells. It can be the result of gallstones, but ultrasounds found no indication of gallstones, or liver or spleen lesions in the girl.
Jaundice can also be caused by viral infections, so the girl underwent blood tests to see if any underlying infection could be the cause of the jaundice and anemia. Blood and genetic tests confirmed the presence of EBV.
The patient lacked the typical signs of infectious mononucleosis: She did not have swollen lymph nodes (cervical lymphadenopathy) or enlarged spleen (splenomegaly), and her fever and sore throat (pharyngitis) were mild. She also had mild liver enlargement (hepatomegaly).
Despite these atypical symptoms, the patient’s peripheral blood indicated infectious mononucleosis showing lymphocytosis — high levels of certain immune cells called lymphocytes — a characteristic sign of infectious mononucleosis.
Blood tests also revealed the presence of auto-antibodies that were reactive against red blood cells at low temperatures (4ºC), which confirmed the diagnosis of cold agglutinin disease.
Considering her fatigue and hepatomegaly, the girl was started on methylprednisolone (a corticosteroid) injections. Her blood and urine values — including hemoglobin, red blood cells, and bilirubin — normalized, and she was discharged from the hospital on the eighth day.
She continued taking oral methylprednisolone, which was eventually discontinued three weeks later. Lab tests continued to confirm normal blood values and negativity for EBV. The patient remained in good health two months after her hospitalization.
The researchers stressed that no antiviral therapy (acyclovir or valacyclovir) was used. Although the patient’s improvement “could have been spontaneous because of the natural history of the disease, methylprednisolone use was safe and likely associated with faster resolution of EBV,” the team noted.
Corticosteroids are not normally recommended for primary CAD, because they do not diminish antibody production. However, they may benefit patients with CAD due to EBV infection, as this case report suggests.





