Report Details How CAD Patient Was Warmed for Hip Surgery
Warming techniques used before, during and after hip replacement
Written by |
Multiple strategies to keep a woman with cold agglutinin disease (CAD) sufficiently warm right before and during hip replacement surgery allowed for a safe procedure and the absence of post-surgery complications, a case study shows.
One way to reduce heat loss — and therefore prevent disease worsening — was to raise the temperature of the cement that is used to fix the artificial bone, known as the implant, that replaces the damaged hip joint.
“Warming strategies and higher temperature of the cement allowed safe perioperative management,” the researchers wrote. The perioperative period includes the moments just before, during, and right after the surgery.
The case report, “Perioperative Management of a Patient With Severe Cold Agglutinin Disease Undergoing Total Hip Arthroplasty With a Cemented Stem: A Case Report,” was published in A&A Practice.
CAD occurs when the body makes cold agglutinins, or antibodies, that bind to red blood cells and cause them to form clumps when the body’s temperature falls well below normal.
The clumped red blood cells then are broken down by the immune system. When this happens, it can cause hemolytic anemia (too few red blood cells due to their fast destruction) and other symptoms.
As such, careful management of body temperature is required when these patients undergo surgery.
“Particular attention must be paid to temperature control in patients with high [levels] of cold agglutinins, since general anesthesia causes hypothermia [lower-than-normal body temperature] … and anesthetic-induced impaired thermoregulation,” the researchers wrote.
Case report from Japan
Now, a team of doctors in Japan reported the case of a 65-year-old woman who was scheduled for a total hip replacement due to osteoarthritis, a condition that causes joints to become painful and stiff.
Since hip replacement usually is done under general anesthesia, the operating room must be kept warm enough before, during, and after surgery to avoid disease worsening in CAD patients.
But replacing a damaged hip joint also requires the use of a type of fixing cement that’s usually kept at a low temperature of less than 25 C (77 F).
“Therefore, it is important to take measures to avoid a decrease in body temperature,” the team wrote.
The woman had been diagnosed with osteoporosis and autoimmune hemolytic anemia due to CAD, for which she was taking daily prednisolone, an immunosuppressive treatment.
Her symptoms included Raynaud’s phenomenon — a condition that causes blood vessels to constrict — that occurred when the skin in her fingertips, toes, and nose turned purple when exposed to cold temperatures.
Every winter, she experienced shortness of breath and her levels of hemoglobin, the protein in red blood cells that carries oxygen around the body, dropped below normal.
“Although we suggested that surgery should be performed when the temperature was warm enough, the patient had unbearable joint pain. Thus, surgery was performed in spring,” the researchers wrote.
Warmed blood transfusion
Before surgery, hemoglobin was still below the normal level, so she received a warmed transfusion of red blood cells to raise her hemoglobin levels.
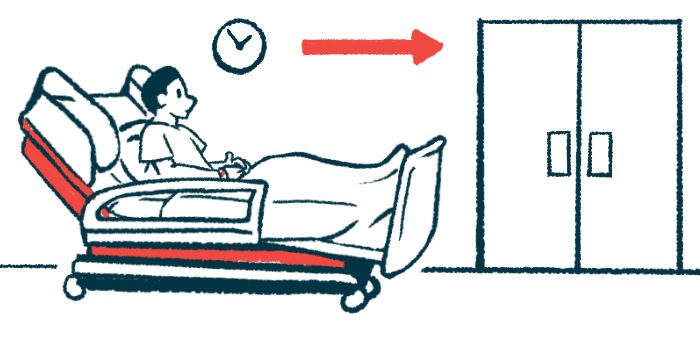
On the day of surgery, the temperature inside the operating room was set at 28 C (82.4 F). On the way from the hospital ward to the operating room, the woman wore gloves and socks and she was covered with blankets.
“Nevertheless, the axillary [armpit] temperature was 35.8 °C [about 96.44 F] when she entered the operating room,” the team wrote.
As such, she continued to wear gloves and socks in the operating room and a forced-air warming system that circulates warmed air around a patient’s body was used to raise her temperature.
Anesthesia was induced only after her armpit temperature reached 36.8 C (98.2 F), and the gas used for anesthesia and breathing was warmed to 38 C (100.4 F). All infusions were heated to 40 C (104 F).
In addition, the cement was maintained at room temperature after the doctors confirmed it could be used at a temperature higher than its usual (lower than 25 C, or about 77 F).
“We used the cement at as high a temperature as possible,” the team wrote, adding that “good cement–bone and cement–implant interfaces were established without any complications, and no hypothermia or hemolysis [red blood cell destruction] was observed after cementation.”
During the surgery, her internal temperature (measured in the esophagus) and her peripheral temperature (measured between the fingers) did not drop below their normal temperature.
The woman lost up to 1.4 liters of blood during the surgery, but a fast administration of a blood transfusion prevented a drop in hemoglobin levels.
“The postoperative course was excellent, and the patient was discharged on postoperative day 11,” the team wrote.






