COVID-19 Triggered CAD, Muscle Inflammation in Leukemia Patient, Report Says
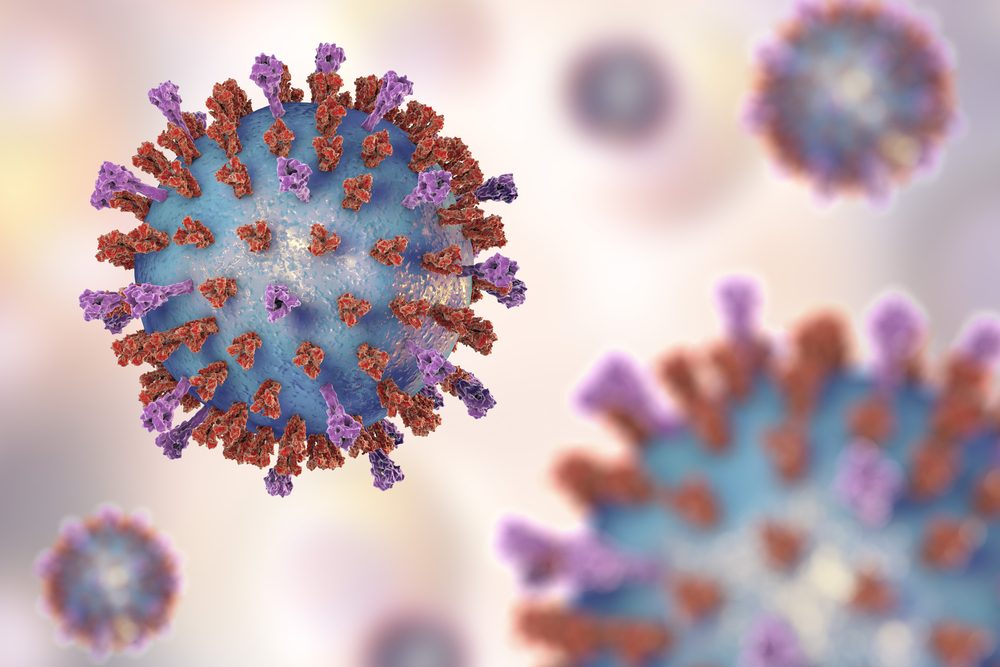
A woman developed cold agglutinin disease (CAD) and myositis (muscle inflammation) as a complication of COVID-19, underscoring the importance of a timely, comprehensive evaluation to identify rare complications of SARS-CoV-2 infection.
Researchers noted that the patient’s history of leukemia and treatment with tirabrutinib, a medication that blocks abnormal immune cell activity in cancer and autoimmune diseases, may have played a role in the development of these disorders.
More study is “required to ascertain the relation between … anemia and myositis with SARS-CoV-2 infections especially in the setting of underlying malignancy,” they wrote.
The case was described in the study, “SARS‐CoV‐2 infection complicated with cold agglutinin disease and myositis,” published in the journal Clinical Case Reports.
CAD is caused by the production of self-reactive antibodies that mistakenly attack and destroy red blood cells at low body temperatures. Secondary CAD, which can be triggered by a bacterial or viral infection, has been reported as a complication of severe COVID-19.
Here, a 69-year-old woman was being treated with tirabrutinib for advanced (stage IV) chronic lymphocytic leukemia, when she contracted COVID-19, complicated by CAD and muscle inflammation.
The patient was diagnosed with SARS-CoV-2 infection, the virus that causes COVID-19, two days after arriving at a hospital in Indiana with a fever, body aches, and a dry cough. A nasal swab for COVID was given at the hospital, and use of tirabrutinib stopped. She was sent home with a prescription for daily treatment with the antibiotic levofloxacin at 750 mg.
A week later, the woman returned to the hospital with difficulty breathing, loss of appetite, and fatigue, and was admitted. She had a low-grade fever of 100.3 F (38 C), a slightly elevated heart rate (99 beats per minute; normal: 60–100), elevated respiratory rate (24 breaths per minute; normal: 12–20), low oxygen saturation (89%; normal: 95–100%), and slightly elevated blood pressure.
A tapered dose of 6 mg daily of the anti-inflammatory corticosteroid dexamethasone was initiated, and she was discharged a week later with a recommendation to remain on supplemental oxygen.
Two days after her discharge, she was again admitted with severe pain in her lower limbs and muscle weakness in the pelvic region. Skin discoloration and lesions consistent with a blood-clotting disorder, as well as severe tenderness and sensitivity to pain, were observed during a physical exam. Muscle weakness was also detected, particularly in the lower limbs.
Blood tests revealed signs of muscle injury or stress, red blood cell damage, and inflammation without any signs of an acute infection. Red blood cell clumping and rupture at temperatures below 30 C (86 F), and structural abnormalities in both red blood cells and immune cells were also observed.
At this point, large and fluid-filled blisters started to form on her lower limbs, accompanied by skin discoloration on her upper limbs.
Worsening platelet counts (11,000/mm3; normal range: 150,000–350,000/mm3) and anemia (hemoglobin 6.7 g/dL; normal: 12.0–15.5 g/dL), prompted treatment with prednisone for four weeks. Four doses of rituximab, and an immunoglobulin infusion were also administered.
The woman stabilized and was discharged to a rehabilitation facility about a month after she first coming to the hospital. Five months later, her skin lesions had fully healed.
“To our knowledge, simultaneous myositis and cold agglutinin disease associated with SARS-CoV-2 have not been previously reported,” the investigators wrote. “Further data [are] needed to direct immunosuppression treatment in patients with [blood-related] complications associated with SARS-CoV-2.”