AIHA Patients at Greater Risk of Thrombotic Events, Report Advises
Physicians should be aware that patients with autoimmune hemolytic anemia (AIHA) are at greater risk of experiencing thrombotic events — blood vessel obstruction driven by blood clots — to better manage their condition, a case report highlighted.
The case study, “Autoimmune Hemolytic Anemia and Pulmonary Embolism: An Association to Consider,” was published in the journal TH Open.
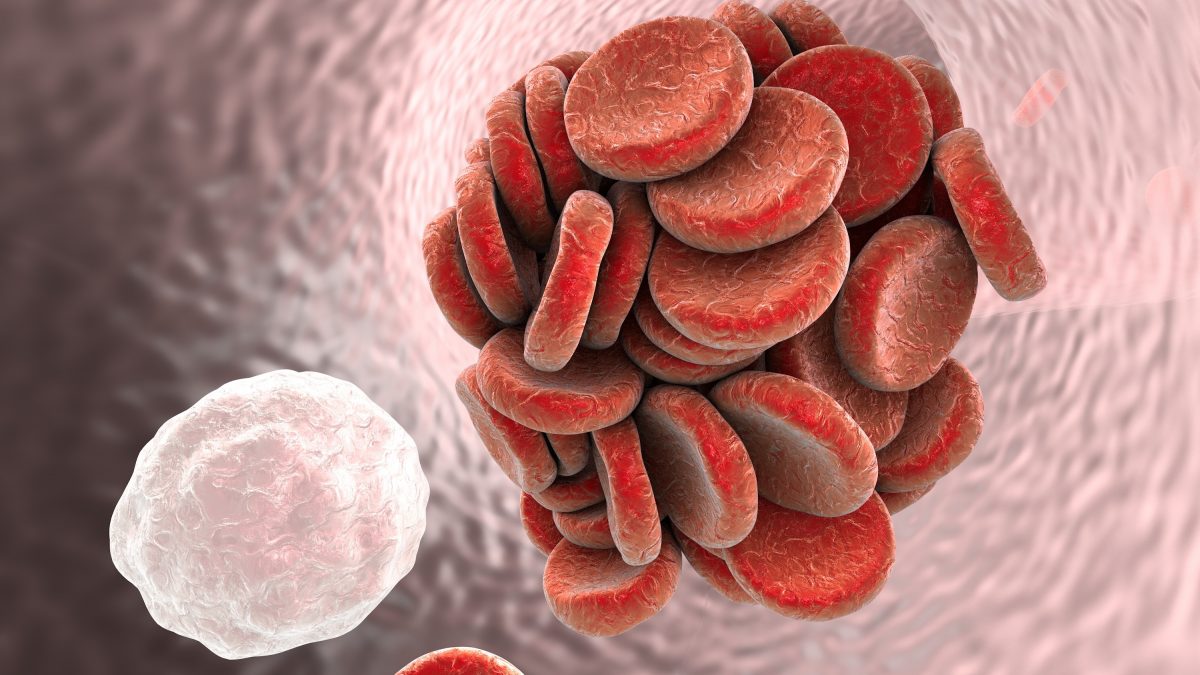
AIHA is caused by antibodies, called agglutinins, that target and destroy the body’s red blood cells. When antibodies bind and destroy blood cells at or above 37 C (98.6 F), patients are said to have “warm AIHA.” In contrast, when they do so at lower temperatures — usually between 0–10 C (32–50 F) — patients are said to have cold agglutinin disease.
AIHA is deemed to be primary when it has no clear cause, or secondary when it is associated with an underlying condition, such as cancer or an infection.
Patients with AIHA are at an increased risk of developing venous thromboembolism (VTE), which occurs when a blood clot forms in a deep vein — usually in the leg, arm, or groin — and blocks blood flow. This can cause patients to have a pulmonary embolism, which occurs when a blood clot that formed in a deep vein travels to the lung and lodges, causing tissue damage and possibly death if untreated.
AIHA patients with other autoimmune disorders, such as rheumatoid arthritis or systemic lupus erythematosus, are at an even higher risk of experiencing VTE.
Despite the close association between AIHA and VTE, guidance on VTE prevention and treatment in AIHA patients is limited, partially due to the rareness of the disorder.
In this report researchers in Switzerland described the case of a 75-year-old man with warm AIHA who developed pulmonary embolism shortly after being diagnosed.
The patient was admitted to the emergency room with severe shortness of breath, which had worsened over the previous four weeks, as well as severe generalized weakness and jaundice (yellowish skin).
He had a history of moderate chronic obstructive pulmonary disease, which was well-controlled, and chronic ischemic heart disease, for which he had undergone double bypass surgery.
Blood tests found multiple signs of hemolytic anemia caused by red blood cell destruction. Specifically, the patient had a hemoglobin level of 83 g/L, which was below the normal range of 133–177 g/L, along with an abnormally high production of immature red blood cells. Of note, hemoglobin is the protein that transports oxygen in red blood cells.
He also had excessively high levels of lactate dehydrogenase (1,530 units per liter (U/L), with normal range being 135–225 U/L), and bilirubin (154 micromole per liter (mcmol/L), of which normal range is 0–21 mcmol/L). Both are markers of red blood cell destruction.
More tests revealed the presence of warm-reactive autoantibodies on the surface of red blood cells circulating in the patient’s bloodstream, while a computed tomography scan also showed he had pulmonary embolism. Based on these observations, physicians diagnosed the patient with primary warm AIHA with concomitant, or simultaneous, pulmonary embolism.
He received a blood transfusion and was treated with a high-dose of oral prednisone (1.5 mg/kg per day).
His anemia was treated further with two intravenous infusions of the corticosteroid methylprednisolone at a dose of 125 mg on day nine. This treatment regimen was complemented by the anticoagulant rivaroxaban, which was given twice daily at a dose of 15 mg for the first 21 days, and then once daily at a dose of 20 mg thereafter.
The patient was discharged from the hospital after 13 days, with instructions to taper corticosteroid treatment and continue taking rivaroxaban while having anemia episodes and for at least three months following discharge.
“To date, no guideline preconizes the introduction of an [anticoagulant preventive treatment] nor the screening of VTE in patients suffering of AIHA,” the researchers wrote.
“However, … it seems reasonable to suggest a high level of suspicion for VTE in patients with AIHA flare and to prescribe anticoagulant prophylaxis [preventive] while the patient is exhibiting frank hemolysis [red blood cell destruction],” they wrote.





